
CHIP insurance plan cheaper than Affordable Care for children with autism
Children with chronic conditions are especially vulnerable to health insurance changes, as they often rely on specialists and medications that may not be covered if they switch plans.
Children with chronic conditions are especially vulnerable to health insurance changes in the United States, as they often rely on specialists and medications that may not be covered if they switch plans. A new study finds that these transitions can leave children and their families financially vulnerable as well.

The research, which examines the spending impact of shifting chronically ill children from the Children’s Health Insurance Program (CHIP) to policies offered on the health law’s marketplaces, found that their families’ out-of-pocket costs would likely rise, in some cases dramatically, following a change to marketplace coverage.
The study comes at a time when health insurance issues are on the front burner in Congress. Republican lawmakers are pushing for fundamental changes to the marketplaces and to the Medicaid program. At the same time, Congress must soon decide whether to extend CHIP when its funding ends in September.
Together the state-federal Medicaid and CHIP programs insure nearly 46 million low-income children in the U.S. CHIP covers children whose family income is low, but too high to qualify for Medicaid. The eligibility levels vary by state. Half of states set the upper income eligibility limit at 255 percent of the federal poverty level or higher — about $52,000 for a family of three.
Both programs provide comprehensive coverage for children, with little or no out-of-pocket cost to families.
Since the passage of the Affordable Care Act in 2010, some policy analysts have advocated moving children who are enrolled in CHIP into marketplace plans and dismantling the CHIP program. But earlier evaluations found, as did this study, that CHIP coverage was better and cheaper than marketplace coverage, says Joan Alker, executive director of the Georgetown Center for Children and Families.
CHIP is much smaller than Medicaid, with more than 8 million children enrolled, roughly 2 million of whom have one of six chronic health conditions, including asthma, attention deficit hyperactivity disorder, diabetes, epilepsy, mood disorders and developmental disorders such as autism, according to the study, which was published in the April issue of Health Affairs.
Stark differences:
Using data compiled from state CHIP programs and marketplace plans for 2016 and healthcare-use data from the federal Medical Expenditure Panel Surveys from 2008 to 2013, researchers simulated the annual out-of-pocket costs for children with any of these six chronic conditions if they were enrolled in CHIP versus one of the plans sold on the marketplaces operated by the federal government.
The spending differences were stark. For every chronic condition and at every income level, cost sharing was higher for children enrolled in marketplace plans than for those in CHIP.
Take the case of asthma, the most common condition that the researchers modeled. For a child with asthma whose family’s annual income was between 100 and 150 percent of the federal poverty level, or about $20,000 to $30,000 for a family of three, annual out-of-pocket spending on deductibles and copays would be $284 in a marketplace plan, compared with $27 in CHIP — a difference of $257. At higher incomes, the out-of-pocket spending differences were greater. Families with incomes between 251 and 400 percent of the federal poverty level, or about $51,000 to $81,000 for a family of three, would pay $1,227 out of pocket annually if they were enrolled in a marketplace plan, but just $84 in the CHIP program — a difference of $1,143.
“The lowest-income families were relatively well protected by cost-sharing reductions” in marketplace plans, says study investigator Amy Davidoff, a senior research scientist in the Department of Health Policy and Management at the Yale School of Public Health. Those cost-sharing subsidies, which reduce a plan’s deductible, copayments and coinsurance, are available to marketplace customers with incomes up to 250 percent of the federal poverty level — about $51,000 for three people. These subsidies are the subject of a lawsuit, however, and their fate is unclear.
As family income rises, however, the gap between the out-of-pocket costs for the two different types of coverage increases and becomes quite substantial, Davidoff says. “For these families, it would be huge barrier.”
About 97 percent of children on CHIP belong to families with incomes below 250 percent of the poverty level.
The deductible — the amount that people have to pay on their own before insurance covers most services — was a significant factor in the cost differences. The average deductible in marketplace plans for families with incomes between 251 and 400 percent of the poverty level was $3,126. None of the CHIP programs for families at that income level had deductibles, the researchers found.
Noting that CHIP has a history of strong bipartisan support, Alker says she is hopeful that it will be extended. “I think it would be very hard for Congress to let CHIP expire,” she says, “and put those children into the marketplace, when according to their leaders it’s about to fold.”
This story originally appeared on Kaiser Health News. It has been slightly modified to reflect Spectrum’s style.
Explore more from The Transmitter
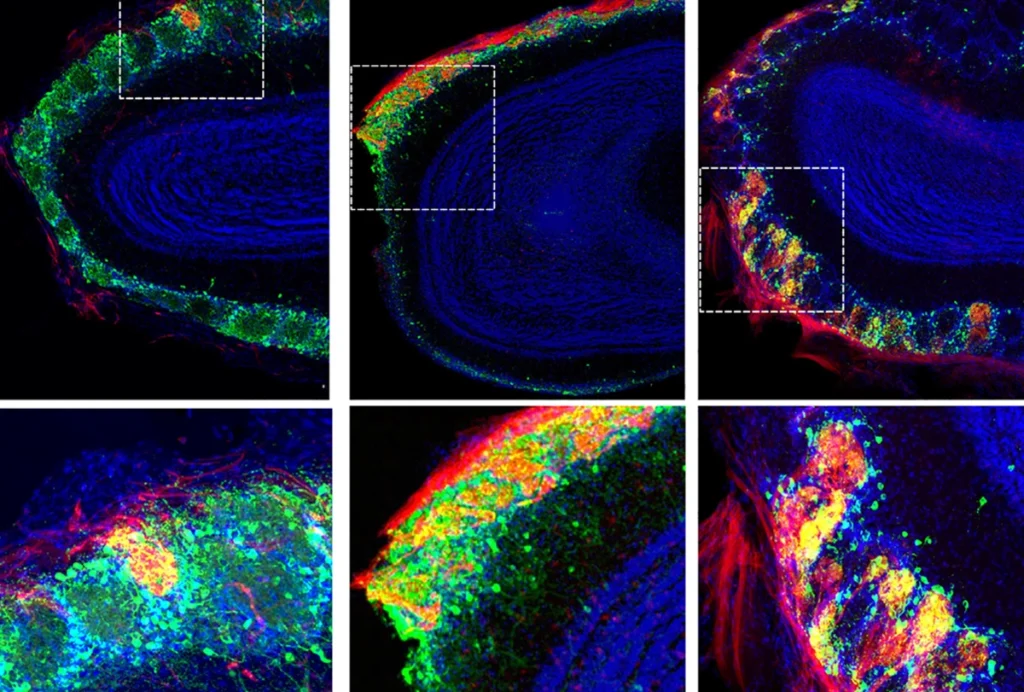
Rat neurons thrive in a mouse brain world, testing ‘nature versus nurture’
