
Infection during pregnancy may alter expression of autism genes
A mother’s immune response to a severe infection during pregnancy disrupts the expression of autism genes in her child, a rat study suggests.
A severe infection during pregnancy disrupts the expression of autism genes in the child, a study in rats suggests1.
The findings may help to explain why maternal infections boost autism risk by as much as 37 percent.
Infections set off an immune reaction involving molecules that can enter the womb. The new work shows that infection in a pregnant rat dampens or boosts the expression of a number of genes linked to autism. Many of these genes control the growth and formation of the junctions between neurons, called synapses. And some are on a list of genes that harbor rare, harmful mutations in some individuals with autism.
“It’s amazing what the correspondences are” between findings in rats and those in children with autism, says Eric Courchesne, professor of neuroscience at the University of California, San Diego, who was the senior collaborator on the study. “Even though there may be different causes behind autism, these different causes seem to converge to common attributes.”
Environmental factors such as maternal infection sometimes exacerbate the effect of genetic risk factors for autism. For example, a 2015 study revealed that children who have a large DNA deletion or duplication linked to autism and whose mothers had infections during pregnancy have more severe autism features than children with only one of these risk factors.
The new work shows how the prenatal environment may affect autism genes to alter brain development, says Melissa Bauman, associate professor of psychiatry and behavioral sciences at the University of California, Davis School of Medicine, who was not involved in the study.
Large overlap:
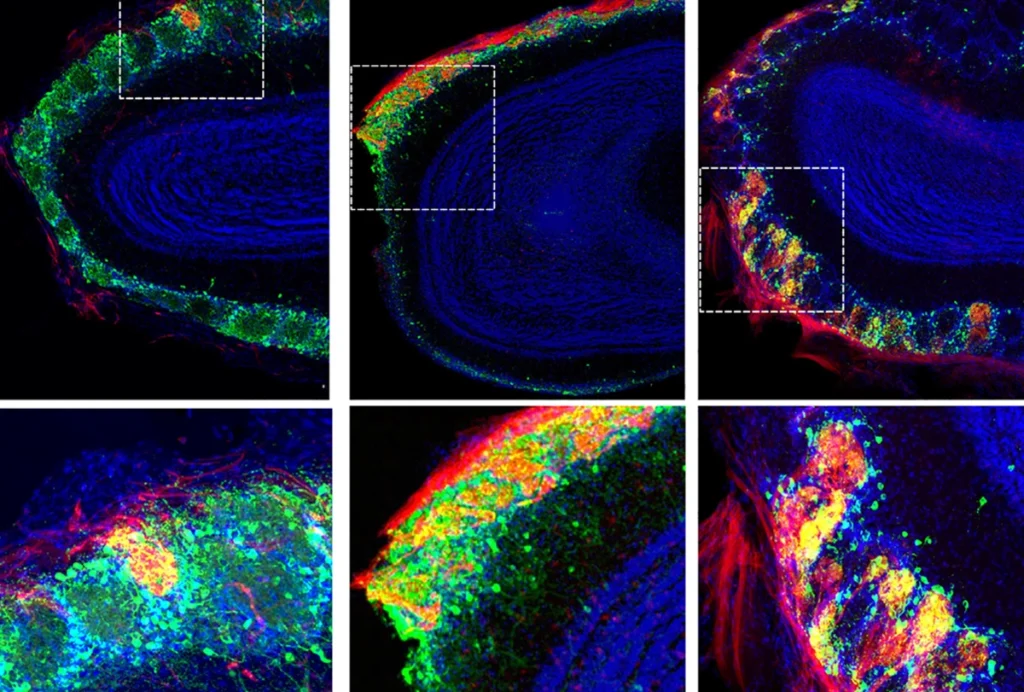
Courchesne and his colleagues used gene expression data from a 2012 study. In that study, researchers injected pregnant rats with a chemical called lipopolysaccharide, which mimics a bacterial infection and elicits a strong immune response. Rat pups exposed to an immune response in the womb are known to show autism-like features, such as social deficits.
In the 2012 study, researchers injected the rats on day 15 of pregnancy, equivalent to the end of the first trimester in people. Four hours after the treatment, they collected the fetal brain tissue to determine which genes were expressed and at what levels.
In the new work, Courchesne team reanalzyed this dataset to confirm previous results and found that the pups express 4,033 genes at unusually high levels. These genes seem to play a role early brain development, guiding processes such as cell division. The pups also show diminished expression 4,959 genes that help guide the formation of neurons and synapses.
The researchers then looked to see if any of 35 autism-linked genes cropped up in the group of 4,959 genes — and found that 20 of them did.
The team also found that immune activation decreases the expression of 75 percent of ‘high-confidence’ autism genes in a database of known autism genes.
The study represents a step forward in understanding how maternal infection might boost autism risk, says Alan Brown, professor of psychiatry and epidemiology at Columbia University, who was not involved in the study. “The findings indeed overlap with several genes and mechanistic pathways that have been suggested in autism,” says Brown.
Time lapse:
Maternal immune activation does not appear to affect the expression of FMR1 or CHD8, two genes with strong ties to autism. But each of these genes is known to regulate hundreds of others, and some of their targets are altered.
The researchers compared their findings with those from studies of postmortem brain tissue from people with autism, and found large networks of genes in common. For instance, a network of genes involved in protein translation is altered in both types of tissue.
But looking at the single-gene level indicates less convergence. Dozens of disrupted genes in mature human brain tissue are similarly changed in rat fetuses, but that is less than 5 percent of the roughly 9,000 genes that Courchesne’s team found altered.
One possible explanation is that some of the genes have functions in early brain development and are not detectable in the mature brain, says Tiziano Pramparo, research scientist at the University of California, San Diego, who led the new study.
The rat model may have limited relevance to people for other reasons. The researchers induce an infection in rats that is much more severe than most of the ones that pregnant women get. “That’s why we see a massive dysregulation of genes,” Pramparo says. “This is not the case with getting a common cold.”
What’s more, various genetic factors as well as the timing of a maternal infection are likely to play a role in which children develop autism, Bauman says. The vast majority of women who have infections during pregnancy do not have children with the condition.
In future studies, the researchers plan to examine gene expression in blood samples of toddlers with autism.
- Lombardo M.V. et al. Mol. Psychiatry Epub ahead of print (2017) PubMed
Explore more from The Transmitter
Rat neurons thrive in a mouse brain world, testing ‘nature versus nurture’
