One morning in late 2018, Monika Fleshner, professor of integrative physiology and a member of the Center for Neuroscience at the University of Colorado Boulder, was at home enjoying a breakfast of two eggs, strawberries and toast when she got a call from Shelby Hopkins, her lab technician. “Moni, the DEA are here,” Hopkins said. “They need to talk to you, and they have guns.”
At the time, Fleshner was testing the effect of CBD oil, a cannabis derivative, on rats’ acute stress response. Marijuana use was legal in Colorado, but the U.S. Drug Enforcement Agency (DEA) classified it under the strictest category, reserved for drugs not accepted for medical use and with a high potential for abuse.
Before starting her investigation, Fleshner had asked the DEA about studying cannabis and was told she needed a Schedule I license, she says. “You mean like for ecstasy and heroin?” she remembers telling the agency. “This is CBD, you know?” She decided to work with low-THC CBD oil instead.
In the end, the DEA confiscated it anyway.
Most cannabis derivatives are still classified as Schedule I drugs, but that might be about to change. Yesterday, the attorney general and the DEA published in the Federal Register a proposal to move cannabis to Schedule III, a less restrictive category.
There is no time frame for when—or if—the agency will formalize it once the 60-day comment period closes, but still, “this is very historic,” says Cecilia Oyediran, chair of the New York State Bar Association Cannabis Law Section. “This is the first time in 50 years, or since the Controlled Substance Act was made in 1970, that the federal government has acknowledged that cannabis has some medical use.”
For scientists, the rescheduling would “make a world of difference,” says Caroline Bass, associate professor of pharmacology and toxicology at the University at Buffalo. She often avoids doing research with cannabis because “it is too hard to get the drugs. And even if you get the drugs, getting the type of drugs you need is very problematic,” she says.
I
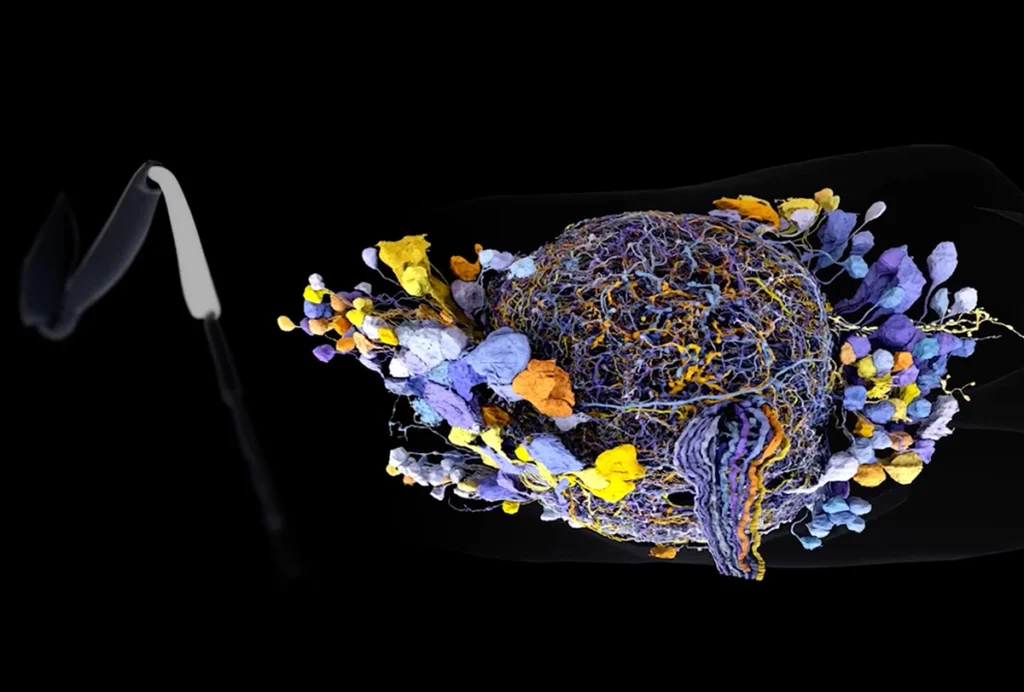
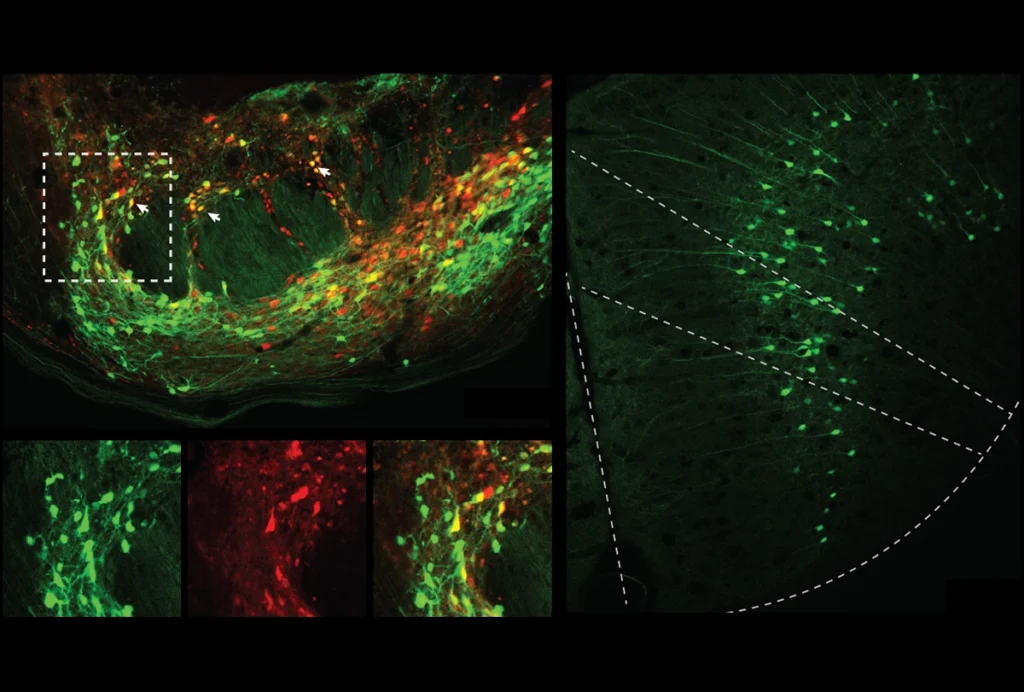
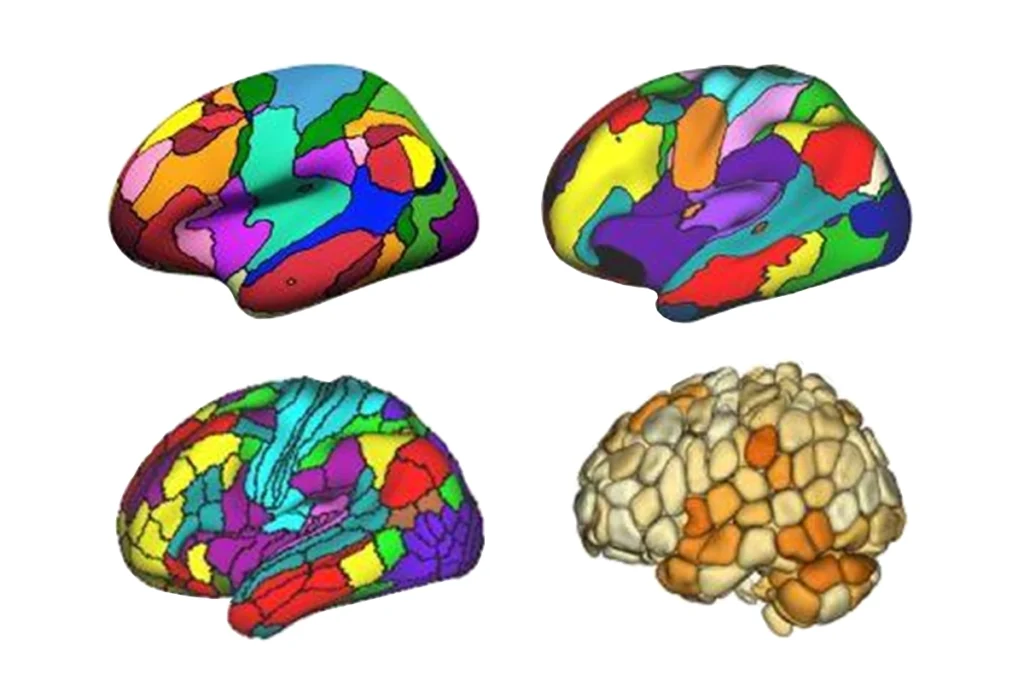
n people, natural endocannabinoids target the body’s two cannabinoid receptors, CB1 and CB2, and the endocannabinoid system also contains enzymes that regulate the production and degradation of endocannabinoids. This system is involved in memory, motivation, hunger regulation, pain and inflammation, and disruptions to it have been tied to some psychiatric disorders, such as schizophrenia.CB1 “is probably the most important modulator” in the brain, says Giovanni Marsicano, professor of neuroscience at the University of Bordeaux. THC, the principal psychoactive component in cannabis, binds to the receptor, offering researchers an opportunity to study how the CB1 receptor and the endocannabinoid system work.
“The reality is that if we didn’t have cannabis, and THC in cannabis in particular, we would have no idea of one of the most pervasive and important modular systems the brain has,” says Daniele Piomelli, professor of neuroscience and director of the Center for the Study of Cannabis at the University of California, Irvine.
But it has not been easy to acquire cannabis for research. And the endocannabinoid system is often neglected in neuroscience coursework, Piomelli says, in part because of the cannabis restrictions. When he started working with cannabis in the 1990s in France, it took a lot of motivation to overcome the restrictions, he says.
“Even in Paris, I could go to the corner of the street and get some pot if I wanted to get high,” he adds, “but as a lab researcher, no, I could not do it.”
I
f the classification change is made into law, one of the biggest differences researchers will see concerns licensing. Institutions can obtain licenses for all of their researchers to use Schedule III drugs, but Schedule I licenses are issued to individual investigators. For instance, under the current classification, Bass could use her university’s Schedule III license to access ketamine, but she would need her own independent Schedule I license to access and study cannabis. She says it’s not impossible to get one, but it can take months. “It’s just literally not worth it,” she says.In 2020, only about 600 researchers in the United States had Schedule I licenses to study cannabis. But the classification change should lead to “an explosion in research for those practitioners that have until now been limited,” says Richard Shain, director of the DEA-approved cannabis provider Maridose.
The classification change should also make it easier for researchers working with cannabis to switch up protocols mid-study. To maintain a Schedule I license, licensees must provide the DEA with research plans and detailed information on how the drug will be used and discarded in advance.
“One of the big pains about the Schedule I license is that it is very specific,” says Pamela Maher, research professor at the Salk Institute for Biological Studies. For instance, if during one of her experiments Maher found a new cannabinoid she wanted to test for its effects on cellular aging, she would need to file an amendment with the DEA and then wait for approval.
Lastly, as a Schedule III drug, cannabis would be easier to obtain. Before 2021, there was only one DEA-authorized vendor of cannabis for research purposes, and its product was called into question by researchers at the University of Colorado in a 2017 Nature paper. It wasn’t until that year that the DEA started accepting applications from other providers. So far, the DEA has approved another six, but more vendors work with Schedule III substances, says Elise Weerts, professor of psychiatry and behavioral sciences at Johns Hopkins University. With the rescheduling, the DEA may also stop imposing quotas on the amount of cannabis that manufacturers can produce, possibly increasing access.
When Maher wanted to study a cannabinoid so low in THC that it is not a scheduled drug, she still found that providers were skittish. “None of the companies I talked to were willing to touch it or to manufacture it because they were afraid,” she says.