Some people in ‘failed’ drug trial for autism showed benefit
An experimental drug called arbaclofen improved autism features in about 13 percent of people who took it in a shuttered clinical trial.

An experimental drug called arbaclofen improved autism features in about 13 percent of those with the condition who took it in a shuttered clinical trial1.
The trial ended in 2012. The new findings, reported a full four years later, suggest that arbaclofen benefits a subgroup of people with autism.
The findings highlight the difficulty in designing clinical trials for a condition as diverse as autism, says Jeremy Veenstra-VanderWeele, who led the trial at one site.
“There seems to be a group of people that benefits [from arbaclofen], but it’s not a huge group,” says Veenstra-VanderWeele, associate professor of psychiatry at Columbia University. “I couldn’t tell you what differentiated that subset [of people], and so that’s one of the real challenges moving forward.”
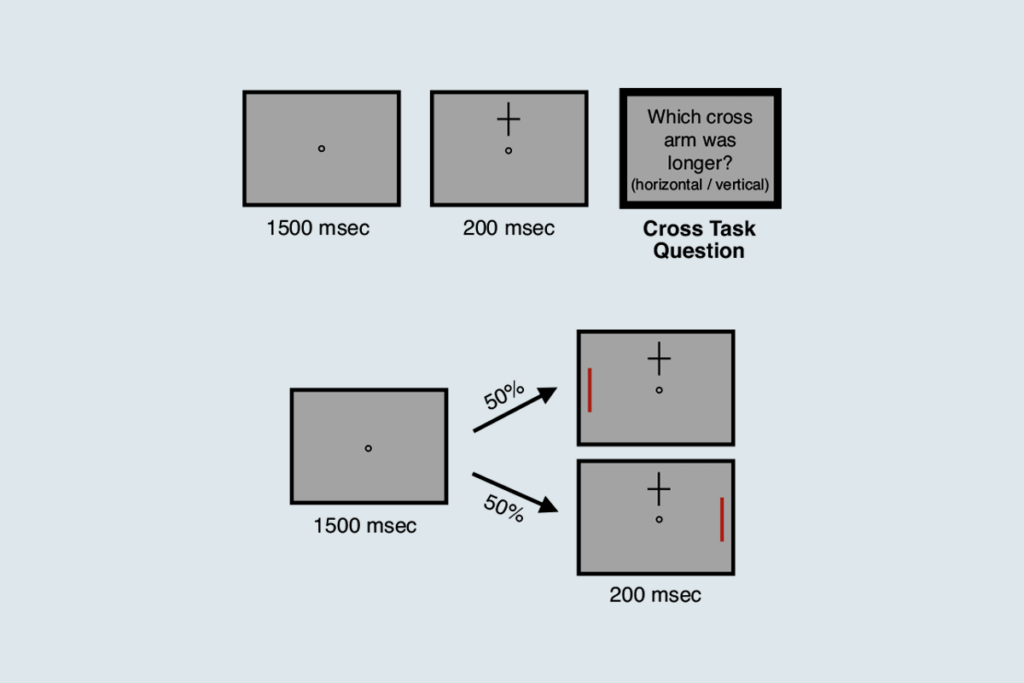
Researchers designed the clinical trial to test the effects of arbaclofen primarily on ‘social withdrawal’ — a tendency to avoid engaging with others — and found no improvement in that measure.
The disappointing result hastened bankruptcy for Seaside Therapeutics, the company that made the drug, and cut short a second trial testing arbaclofen in people with the related fragile X syndrome. But many parents of the trial’s participants insisted that arbaclofen helped their children. More than 5,000 people petitioned government agencies, pharmaceutical companies and investors to continue testing the drug.
The new findings, published 9 November in Neuropsychopharmacology, validate the parents’ observations. Of the 76 participants who took the drug, 10 improved more than those who took a placebo, according to a measure that is based on a clinician’s overall impression of the participants.
Promising signs:
Arbaclofen enhances brain signals that dampen neurons’ activity. This may restore balance between excitatory and inhibitory signals in the brains of people with autism or fragile X syndrome.
But only some people with autism may have a signaling imbalance to begin with, says Randi Hagerman, medical director at the University of California, Davis MIND Institute.
“You can’t expect something to cure 100 different forms of autism in one fell swoop,” says Hagerman, who led one of the sites involved in the fragile X trial.
The U.S. Food and Drug Administration requires clinicians to pick the primary measure of a clinical trial before the trial begins. For arbaclofen, the goalpost was social withdrawal, as measured by a parent questionnaire called the Aberrant Behavior Checklist. By this measure, the 76 people taking the drug did not significantly differ from the 74 people given a placebo pill.
The researchers also recorded a clinician’s general assessment of the participants, called the Clinical Global Impression Scale. This measure indicated an overall benefit from arbaclofen, but the result stemmed mainly from the small subgroup who improved.
“The provocative Clinical Global Impression findings warrant follow-up in another study and some further exploration into why it differed so much from the other measures,” says Joseph Piven, professor of psychiatry at the University of North Carolina at Chapel Hill, who was not involved in the study.
Careful testing:
The researchers used a third test called the Vineland Adaptive Behavior Scales, weighted to evaluate social behavior. The test rates caregivers’ and clinicians’ impressions of how well the participant interacts with others before and after the trial. Ideally, the same clinician and caregiver complete both assessments, but this did not always happen in the trial.
The researchers found no overall difference between the arbaclofen and placebo groups on this measure. But when they narrowed their analysis to the 97 individuals who were rated by the same people before and after the trial, they found that arbaclofen improved the participants’ ability to socialize.
The findings suggest that only some people with autism benefit from arbaclofen. Alternatively, the trial measures may detect improvements in only a subset of people, says Veenstra-VanderWeele. For instance, only children who speak may be able to convey enhanced interest in socializing within the time frame of the study.
The results also suggest decisions made in the design phase of a clinical trial can make or break the trial.
“There is a science to figuring out how to do these studies, and we’re going to have some failures, in some cases spectacular failures, in order to figure out what does and doesn’t work,’ he says.
After Seaside Therapeutics went out of business in 2013, the Simons Foundation purchased the rights to arbaclofen. (The Simons Foundation is Spectrum’s parent organization.) The foundation intends to pursue clinical trials in people with autism and is also making the drug available to qualified researchers.
References:
- Veenstra-VanderWeele J. et al. Neuropsychopharmacology Epub ahead of print (2016) PubMed
Recommended reading

INSAR takes ‘intentional break’ from annual summer webinar series
Dosage of X or Y chromosome relates to distinct outcomes; and more
Explore more from The Transmitter
Xiao-Jing Wang outlines the future of theoretical neuroscience
Memory study sparks debate over statistical methods