Unmasking anxiety in autism
Anxiety can assume unusual forms in people with autism — turning uncertainty, or even a striped couch, into a constant worry. New tools may help identify these hidden fears.
N
o one except Gregory Kapothanasis knows exactly what upset him today. On this hot day in July, he went to his day program for adults with developmental disabilities, as he has done without incident five days a week for the past four years. But then things unraveled. According to the program’s report, he grabbed a staff member’s arm hard enough to bruise it. Then, on the bus during the daily outing, he started screaming and hitting his seat. Now, several hours later, he is finally home, but there is a stranger in his living room. Bouncing from one couch to another, clutching a faded beige blanket stolen from his aunt’s dog, Kapothanasis still seems out of sorts.His mother, Irene — who has cared for him, with the help of home aides, for all of his 24 years — is playing over the day’s events, trying to figure out what triggered him. His outburst is disturbingly reminiscent of a difficult period that peaked six years ago but is uncharacteristic of the young man today. Kapothanasis loves interacting with other people, going to the beach and dining at DiMillo’s, a floating restaurant in a decommissioned car ferry in Portland, Maine.
Kapothanasis has autism and speaks only a few words: He can’t explain what happened this morning. Did he have constipation and discomfort, as his doctor suggested? Did he get bored of the day’s program, causing him to act out? Had something occurred on the bus previously that made him fear that part of his day? All his mother can do is wonder — and try to make his evening better.
Kapothanasis places several pieces of gum in his mouth, something his mother says soothes him. Then he curls up for a nap and dozes off. The time it takes him to calm down is short compared with the protracted meltdowns that routinely overtook him during his teen years. He became aggressive starting in puberty: He would bite and hit himself, or hit and grab other students, teachers and bus drivers. His mother had to supervise his interactions with his siblings, even though, as triplets, they had always been close. In December 2011, when he was 18 years old and over 6 feet tall, his behaviors had escalated so much that his school enrolled him at the inpatient clinic at Spring Harbor Hospital in Maine.
“Look, we all have scars from Gregory, we’ve all felt his wrath. And it came to the point where he had to be institutionalized,” his mother says. He spent five long weeks at the hospital. “It was probably one of the darkest moments in our lives,” she says.
When Kapothanasis arrived at the hospital, he didn’t seem sad, cried only on occasion and didn’t respond to things not visible to others — signs he did not have depression or psychosis. But he startled easily, paced and rocked in place, and sweated heavily. “The phrase ‘cat on a hot tin roof’ was pretty descriptive,” recalls Matthew Siegel, director of the developmental disorders program at the hospital.
After several weeks of close observation, Siegel and his colleagues managed to piece together Kapothanasis’ behaviors into a clear diagnosis, based on criteria outlined in the “Diagnostic and Statistical Manual of Mental Disorders.” In addition to his autism, “he was kind of screaming anxiety — if you’re looking for it,” Siegel says. Until then, it seems no one had been. When Kapothanasis entered the clinic, he was on his third antipsychotic medication. Some are approved to treat aggression as a feature of autism, but none treat anxiety. “It’s fair to say that he was not being treated for anxiety,” Siegel says.
There are many reasons it took nearly six years for Kapothanasis to get the help he needed. Doctors may have assumed that his aggression and tendency to hurt himself were part of his autism, Siegel says. Traits that characterize autism — including social deficits, stereotyped movements and restricted interests — can mask or mimic symptoms of anxiety. During a visit to an outpatient clinic, for example, Siegel points out a nonverbal young woman with autism who repeatedly traces a pattern in the air with her hands. At first glance, her gestures resemble ‘stimming,’ the repetitive behaviors often seen in autism. But she does it at specific times, Siegel says, suggesting a ritual related to obsessive-compulsive disorder — a form of anxiety.
Compounding the problem, many people on the spectrum, like Kapothanasis, cannot tell their caregivers or doctors what they are feeling or thinking. Those who can may still struggle to identify and understand their own emotions — a phenomenon called alexithymia — or to articulate them to others. Because of these factors, the clinical questionnaires designed to ferret out anxiety traits in neurotypical individuals are woefully inadequate for many people with autism. The tests may also miss children with autism, who can have unusual phobias, such as a fear of striped couches or exposed pipes.
“People on the spectrum have really unique, distinct ways of perceiving the world, and also have distinct experiences, which is why we’ll see classic things like social phobia and generalized anxiety, but also maybe these more distinct, more autism-related manifestations,” says psychologist Connor Kerns, assistant research professor at the A.J. Drexel Autism Institute in Philadelphia. Kerns and others are working on new ways to measure both ordinary and unusual forms of anxiety in people with autism. This work could help clinicians better detect the anxiety that hides behind autism, reveal the underlying mechanisms and lead to better treatment.
”“We have more to offer the treatment of anxiety right now than we have for the core features of autism.” Lawrence Scahill
Hiding in plain sight:
A
nxiety may seem to be a prominent feature of autism, but it is not one of the diagnostic criteria. “People say, ‘Oh, it’s just part of autism, everyone with autism has anxiety.’ That is 100 percent not true,” Siegel says. “I’ve got 12 kids sitting outside my door at my hospital right now, and several of them do not have anxiety.”Studies attempting to pin down the proportion of people with autism who also have clinically significant anxiety have produced a staggeringly broad range, from 11 to 84 percent. The discrepancy in these reported rates is “fundamentally unbelievable,” says Lawrence Scahill, professor of pediatrics at Emory University in Atlanta. “Whenever you see a range like that, you know that it’s driven by the source of the sample, where they got the sample from, the methods used to do the assessment and how quick they were to pull the trigger on a diagnosis.”
What is believable, he says, is that autism and anxiety are not independent conditions that sometimes co-occur. In fact, children with autism may be inherently more likely to develop anxiety than their typical peers. But the overlap in features between the two conditions makes diagnosing anxiety extremely difficult. “I’m convinced that the measurement of anxiety in children with autism has to be different,” Scahill says.
The traditional tests for anxiety, such as the Screen for Child Anxiety-Related Emotional Disorders and the Spence Children’s Anxiety Scale, rarely hold up as well in children with autism as they do in the groups they were designed for. In a 2013 study, Scahill and his colleagues investigated one particular test — the 20-item anxiety scale of the Child and Adolescent Symptom Inventory (CASI) — in parents of 415 children with autism.
How the researchers framed the test’s questions significantly affected how the parents responded. Less than 5 percent of the parents endorsed statements describing anxiety that require a child to express herself — for instance, “worries about physical health” or “complains about feeling sick when separation is expected.” By contrast, parents were most likely to agree with statements that rely on their observations, such as “acts restless or edgy.” This trend was especially true among parents whose children have intellectual disability.
Based on their findings, Scahill and his colleagues decided to talk to parents as part of their efforts to develop a measure of anxiety specific to children with autism. Over the course of six focus groups, which yielded more than 600 pages of transcripts, the researchers interviewed the parents of 45 children who have both autism and anxiety. They encouraged the parents to describe their child’s behaviors rather than make inferences about what the child was thinking. They then used these observations to formulate 52 questions. The trick to deciding which questions to ask, Scahill says, was not letting features of autism “leak” into them. Many parents talked about meltdowns but, when pressed for more detail, agreed they couldn’t tell the difference between meltdowns caused by anxiety and those that crop up for other reasons related to autism. Using meltdowns to flag anxiety in children with autism would have been a mistake, Scahill says. Instead, the focus group responses pointed to new indicators, including “Gets stuck on what might go wrong” and “Needs a lot of reassurance that things will work out.”

In unpublished data, the researchers combined the 52 new questions with the 20 questions on the CASI and gave them to 990 parents of children with autism. Based on the responses, they weeded out 31 items that were either redundant, seemingly irrelevant or rarely endorsed by the parents. Based on the remaining 41 queries, they found that roughly one-quarter of the children in the study have high levels of anxiety, another quarter have low levels of anxiety, and the rest fall somewhere in between.
The researchers plan to test whether the measure is reliable over time, evaluating the same children with 10-day breaks between sessions. If the screen proves reliable, Scahill says, it might also be used to assess the efficacy of anxiety treatments in children with autism. “We have more to offer the treatment of anxiety right now than we have for the core features of autism,” he says. “So it behooves us, in my opinion, to be tough-minded about making sure we’re measuring anxiety and not something else.”
Into the unknown:
E
rik Chaston, a 29-year-old graduate of Brigham Young University in Provo, Utah, works at a credit union, developing detailed workflows for the bank’s employees. Chaston, who has autism, has won awards for his clear and surprisingly entertaining videos that elucidate the supply-chain process. But for years, he was also fixated on the faint clicking noises people make with their saliva when they talk.As a student, while working as a sound engineer for the campus sports channel, Chaston began obsessing over fixing these and other sounds in his recordings. “It made me feel like I was constantly worried about things, because everyone talks like this,” he says. He held it together and excelled at work, but would shut down around his family. After he graduated, the problem seeded fears about what kind of job he would be able to hold down. The uncertainty made him especially anxious, he recalls.
This intolerance of uncertainty is a common refrain among people with autism and their parents. For many people on the spectrum, this feeling may simply be an expression of one of autism’s core features — for instance, it may relate to inflexibility in the need to have enough time for a special interest or a fixation. But if that fixation turns into a source of constant fear or worry, it may in fact be an expression of anxiety, researchers say. “To me, it makes a lot of sense that it’s something about the sticky element of the brains of people on the spectrum that would also lead them to have anxiety about change,” Kerns says.
In 2014, Kerns and her colleagues developed an adapted version of the Anxiety Disorders Interview Schedule (ADIS) — a one- to two-hour clinical interview with both parents and children, designed to flag anxiety. Based on interviews with 59 children who have autism and their parents, the researchers documented examples of anxiety that don’t fit the standard definition. Although nearly half of the children had traditional forms of anxiety, 18 of them also showed signs of non-traditional anxiety; another 9 children showed only the unusual forms of anxiety, such as an intolerance of uncertainty.
So Kerns and her colleagues expanded their ‘ASD-specific addendum’ to flag non-traditional anxiety traits that the standard screen might miss: fear of novelty or uncertainty; fear of social situations for reasons other than social ridicule; excessive worry about being able to engage in a special interest; and unusual phobias. The section on fearing change asks, for example, “Does your child react if the change is positive (e.g., getting out of school early)?” The addendum also includes questions about a child’s social skills, sensory sensitivities and repetitive behaviors to help clinicians differentiate anxiety from autism features. For instance, it asks about a child’s history with bullying or social rejection to clarify whether a child is avoiding social events for a good reason — because her bully might attend — or because she is so traumatized by bullying that she fears any social outing. Only the latter would qualify as anxiety. “We want to look for when anxiety has overgrown the actual threat,” Kerns says. Her work solidifies what many clinicians knew anecdotally. “[Kerns] put a description to something that we had been seeing but didn’t have a word for,” Siegel says.
Why a fear of the unknown is a strong feature of autism is less clear. Some researchers speculate that people with autism have trouble predicting future events, heightening their sense of uncertainty. Other work implicates sensory sensitivities and poor verbal comprehension, suggesting that different aspects of autism feed into this type of anxiety.
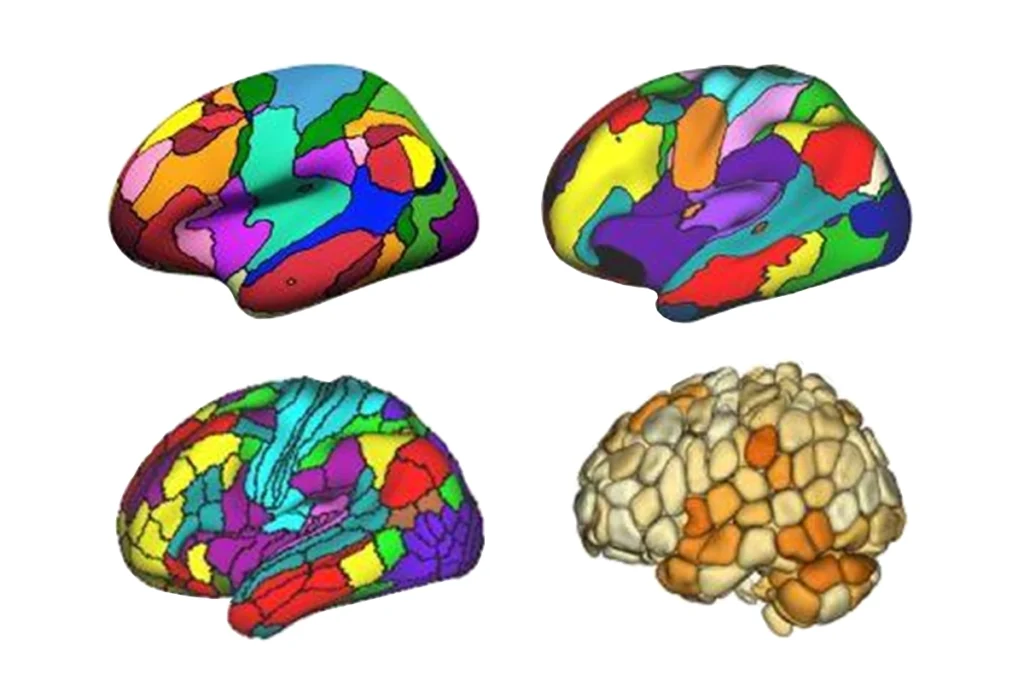
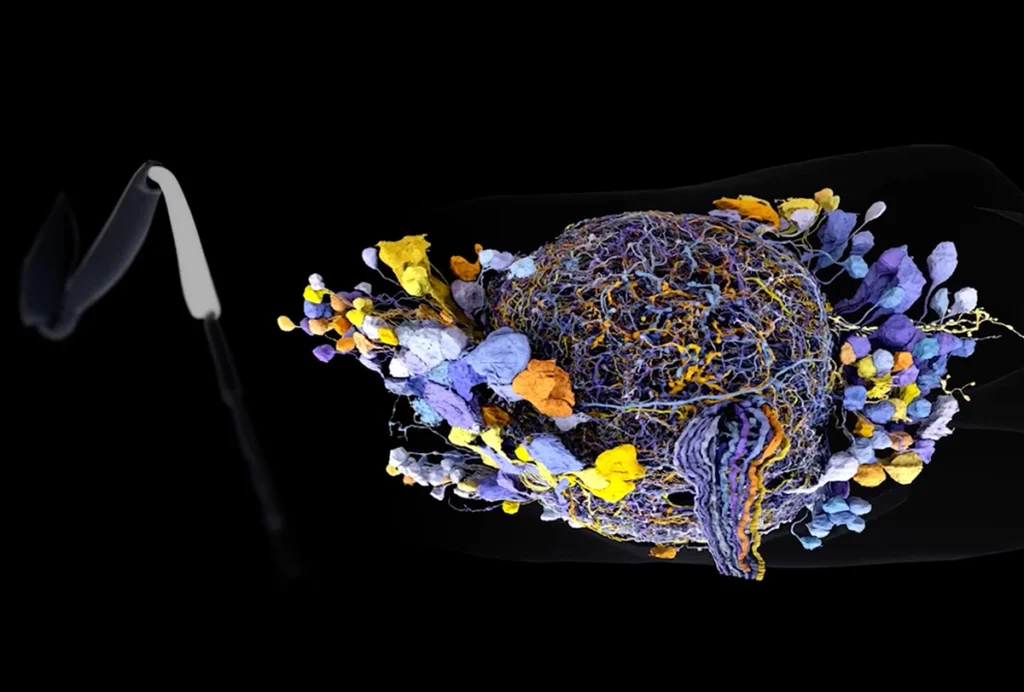
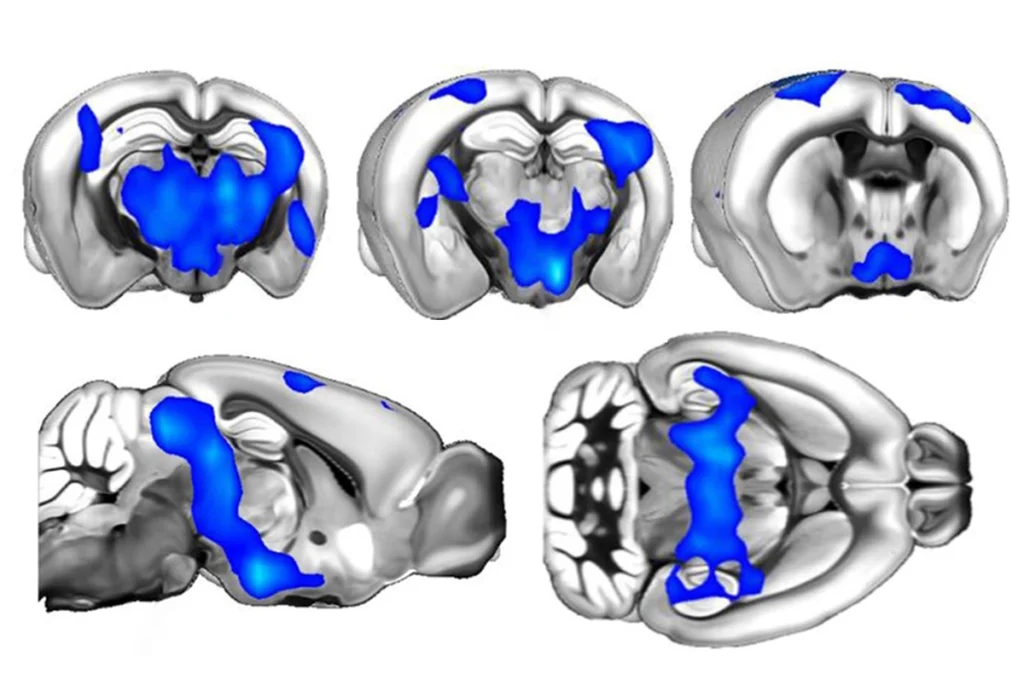
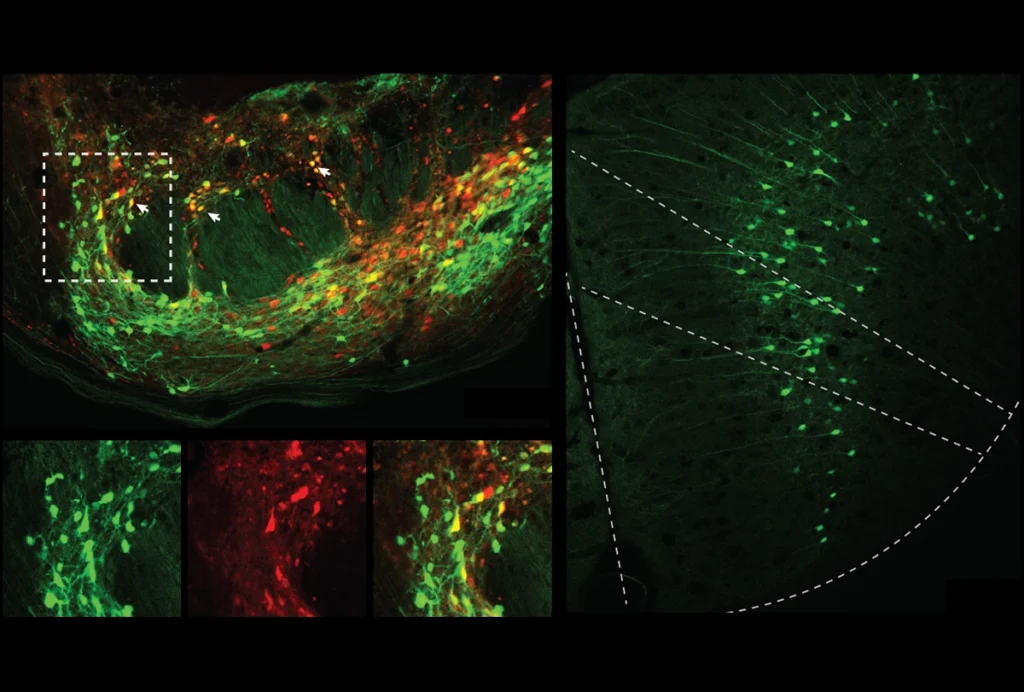
Scientists are also looking for less subjective ways to measure anxiety in autism using various physiological and brain-imaging methods. John Herrington at the Children’s Hospital of Philadelphia and his colleagues are in the midst of a long-term study of 150 children, roughly half of whom have autism, looking at measures of stress, such as heart rate variability and sweat levels. They are also using a technology that tracks where someone is looking to try to distinguish a lack of social interest from social anxiety. Initial findings from their brain-imaging data suggest that the amygdala, a brain region involved in making fearful associations, is smaller in children with autism and anxiety than in those with autism alone.
Another team is also homing in on the amygdala. Mikle South’s team at Brigham Young University is exploring the theory that instead of having an overactive fear response, people with autism have trouble finding a ‘safe space’ and, as a result, are afraid of everything. To test that idea, he is interviewing some adults with autism about their specific fears and scanning others’ brains. More than half of the people he talks to are consumed with worry, he says. “They worry about so much all of the time, they worry about everything,” South says. “There’s nothing they’re not worrying about.”
”“We see social phobia and generalized anxiety, but also more distinct autism-related manifestations.” Connor Kerns
Confronting fears:
B
reaking the cycle of fear is never easy, but it may be especially difficult for someone with autism. For Chaston, help came from what he considered an unexpected source — a self-help book on mindfulness that his mother foisted on him. Practicing mindfulness helped him develop strategies to deal with things that annoyed him. The best-documented approach for treating anxiety in children with autism, cognitive behavioral therapy (CBT), works on similar principles. CBT combines talk therapy with repeated exposures to the source of the fear to change unhelpful thought patterns and behaviors.That said, many children with autism may not benefit from traditional forms of CBT, says Eric Storch, professor of psychology at the University of South Florida in Tampa. Storch’s team has found that children with autism who benefit from CBT do not always maintain those gains: Those who improve only a little sometimes do much better one to two years later, whereas some of those who respond well later relapse. “It wasn’t sticking the way we would predict,” Storch says. The findings suggest that children with autism need therapy for longer, and with more follow-up, than their typical peers — “a critical difference in the treatment approach,” he says.
Children with autism also have trouble generalizing lessons learned in therapy to other aspects of their lives. That means it is especially important to include their caregivers in treatment, because these adults can reinforce the lessons throughout the child’s day, Storch says.

To incorporate some of this extra support, a team at the University of California, Los Angeles developed a modified version of CBT, called the Behavioral Interventions for Children with Autism. The revision recommends, for example, that doctors and parents help a child to master appropriate social behaviors before putting the child in a feared social situation. Confronting situations that make the child anxious is crucial to the therapy’s success, Storch says. The modification also offers extra help for children who may feel socially isolated, having therapists work with schools to give these children peers who can guide them through social situations.
A small 2009 trial suggested that anxiety levels in most children with autism abate after they receive this modified version of CBT. A follow-up analysis found that another version of CBT adjusted for adolescents with autism is just as effective. A team of researchers, including Storch and Kerns, plans to compare the modified version with other therapies in children with autism in a 16-week trial of 180 children. Children who have autism and clinically diagnosed anxiety will receive either the modified or the traditional form of CBT, or will continue with whatever treatment they received before.
Their parents will also take the ADIS, along with Kerns’ addendum. It is possible that the children who have non-traditional anxiety will benefit the most from a modified treatment, Kerns says.
However successful, CBT cannot be the only option for children with autism, notes Roma Vasa, a child and adolescent psychiatrist at the Kennedy Krieger Institute in Baltimore. “There’s a lot of variability in how much they can really report on their internal experience and how connected they are with their thoughts and their feelings,” she says. “There needs to be more trials of effective medication to help these kids.”
There are no drugs approved for treating anxiety in autism. Last year, Vasa and her colleagues published a set of recommendations for clinicians who prescribe anxiety drugs to children on the spectrum. Among her guidelines: Raise doses slowly, as these drugs may exacerbate irritability.
In Kapothanasis’ case, drugs to treat his anxiety, including fluoxetine and guanfacine, turned out to be extremely helpful. Still, Siegel’s team didn’t rely on medications alone to treat him. They discovered that Kapothanasis had no real means of communicating. His aides at school had told his mother that he could, for example, ask for a bottle of water by handing over a drawing of it. But the speech-language pathologists in the hospital realized he really had no idea how to use this picture-exchange system. They helped him learn a new system, in which he points to photos of things from his daily life rather than to cartoon depictions of them. They prepared a visual schedule that lets him know what to expect each day. And, perhaps most valuable, according to his mother, is that they found new ways for him to soothe himself: by bouncing on a yoga ball or running his hands through tubs of uncooked rice.
These tactics are ones that now, years later, can still turn a bad day around. When Kapothanasis wakes from his catnap, he ambles over to the kitchen and makes himself a snack. Back in the living room, he spots a blue fleece blanket his mother has laid out for him in front of the television, a plastic bowl filled with uncooked rice in the center.
As he walks over to the rice, the tension in the air thins palpably. Contorting his large body into a pretzel shape and leaning close to the blanket, Kapothanasis dumps out the container’s contents. Then, carefully placing the bowl in front of him, he scoops up handfuls of rice and lets them fall through his fingers in soft streams down his forehead. The grains tap out a staccato beat as they land in the bowl. Once it is full, he empties the bowl and begins again. And again … and again. After a while, he looks up, faces the stranger in the room for the first time. And smiles.
This article was republished in Scientific American.
Recommended reading

Building an autism research registry: Q&A with Tony Charman
CNTNAP2 variants; trait trajectories; sensory reactivity
Brain organoid size matches intensity of social problems in autistic people
Explore more from The Transmitter
Cerebellar circuit may convert expected pain relief into real thing