The autism traits of people with Dravet syndrome, a rare form of epilepsy, may stem from a certain type of inhibitory cell in the brain, according to a new study in mice. The findings add to a body of work pinning particular aspects of the condition to specific cell types.
Dravet syndrome affects approximately 1 in 15,700 babies and is usually caused by mutations in the gene SCN1A, which encodes part of a sodium channel that is essential for interneurons to initiate and propagate signals. These neurons suppress activity in other neurons.
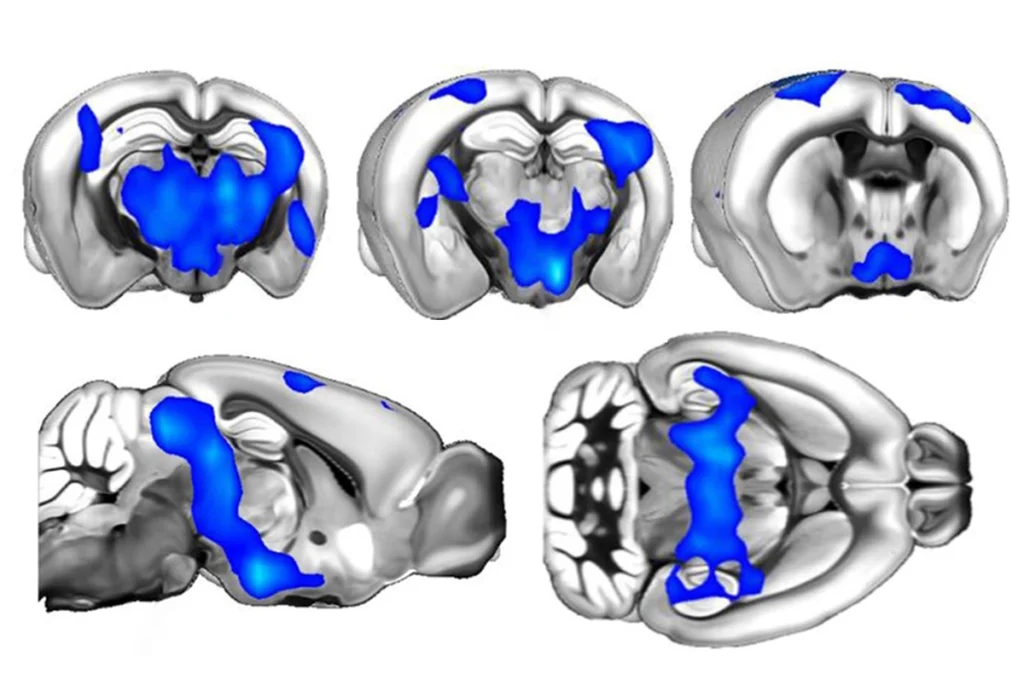
Knocking out SCN1A in inhibitory neurons in the forebrains of mice leads to hallmarks of Dravet syndrome, including spontaneous and heat-induced seizures — some of which are deadly — as well as cognitive and behavioral deficits, according to a 2012 study.
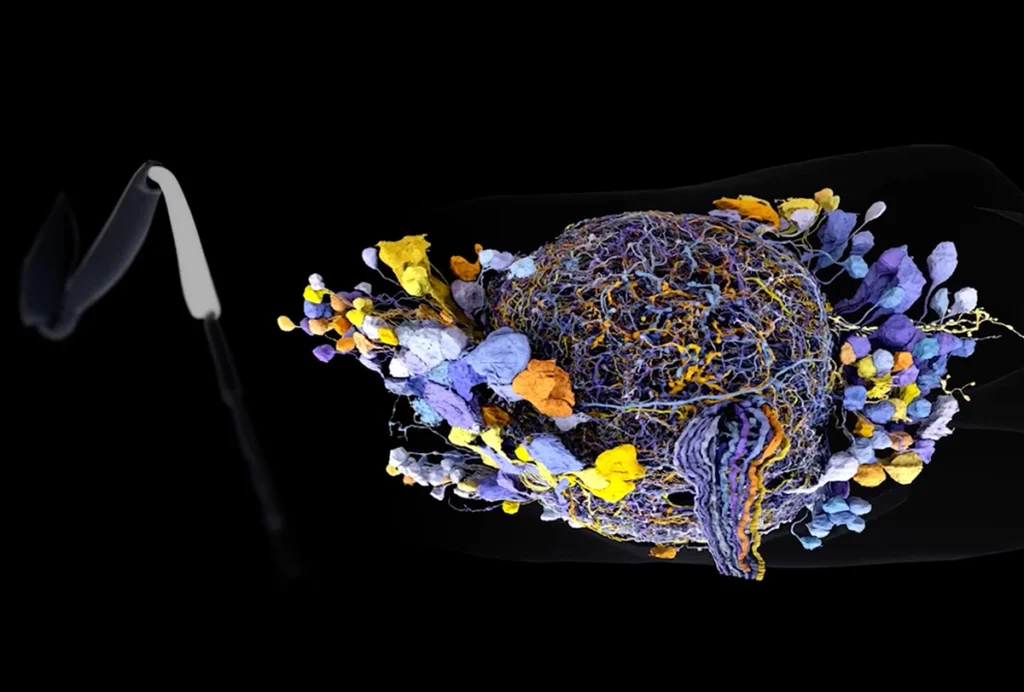
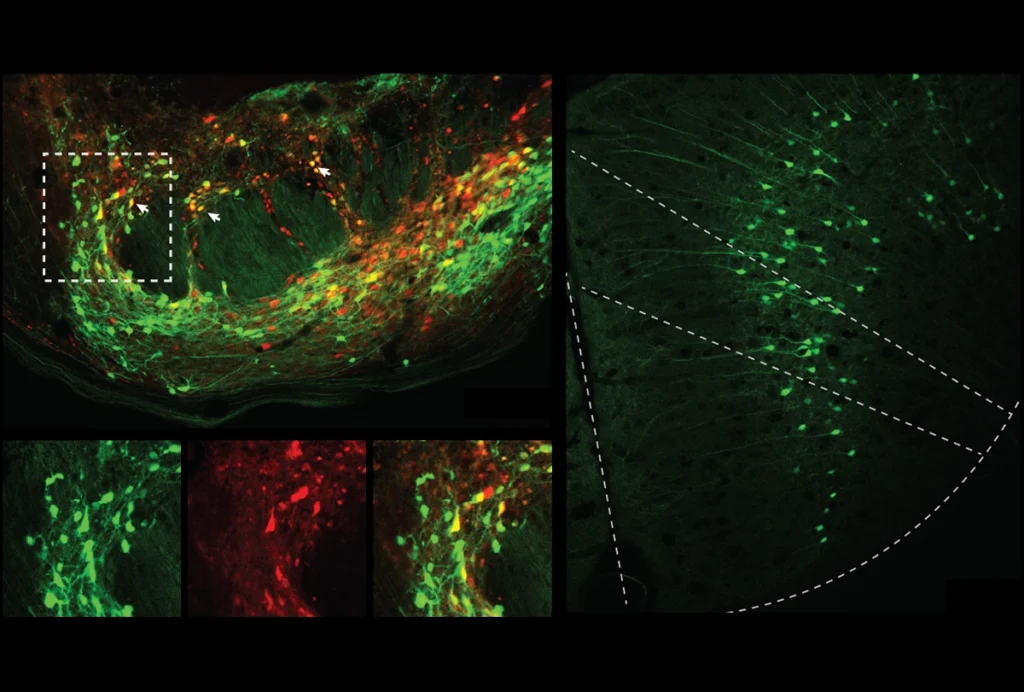
When mice lack SCN1A only in vasoactive intestinal peptide interneurons, or VIP interneurons, these neurons misfire in a specific context, the new work shows: when the mice transition from rest into movement. These mice don’t have seizures, but they do show social differences that parallel autism traits. Unlike other types of interneurons, VIP interneurons suppress the activity of other interneurons, which allows excitation to occur.
The results help explain a mystery about Dravet syndrome, says lead investigator Ethan Goldberg, associate professor of neurology and neuroscience at the Children’s Hospital of Philadelphia in Pennsylvania. People with Dravet experience seizures, so it would seem that hyperexcitability in the brain is key to the syndrome, he says. But that can’t be the whole story, Goldberg says: “If you think about it, it doesn’t really make sense; 99.9 percent of the time, [the person] is not having a seizure.” Plus, people with Dravet tend to have fewer seizures as they reach adulthood.
SCN1A is strongly linked to autism; about 40 percent of people with Dravet syndrome have autism, and many others have at least one autism trait. Goldberg and his colleagues therefore suspected that different mechanisms underly autism traits and seizures in people with Dravet, even if both are disrupted by the same mutation. Dysfunctional firing in VIP interneurons, which would lead to less excitability in the brain overall, could explain the paradox.
“It’s a very interesting story, and I have to say it’s very well done,” says William Catterall, professor of pharmacology and neuroscience at the University of Washington in Seattle, who was not involved in the new study. The lack of seizures in these mice “is a negative result, but it’s a surprising result. It highlights how specific the roles of these interneurons might be.”
O
ver the past decade, researchers have been elucidating the underlying mechanisms of Dravet in detail.Deleting one copy of SCN1A in the mouse forebrain reduces the activity of two types of inhibitory interneurons: hippocampal interneurons and cerebellar Purkinje cells, Catterall and his colleagues reported in 2012. The mice show some autism-like traits, such as a lack of interest in other mice.
Removing the gene specifically from another two types of inhibitory neurons — those that express the chemicals parvalbumin and somatostatin — makes mice more susceptible to thermally induced seizures, Catterall’s team found in 2015. Omitting it in just the former type leads to autism-like behaviors, and in the latter type results in hyperactivity.
When mice lack SCN1A only in fast-spiking parvalbumin-expressing interneurons, they tend to die early in life from seizures because these interneurons don’t allow signals to propagate fully, Goldberg and his colleagues found in 2022. In mice that survive longer, this malfunctioning — and the seizures — disappear.
By contrast, in the new work, mice missing SCN1A in just VIP cells no longer have epilepsy, and they don’t show the hyperactive behavior seen in Dravet model mice, which lack one copy of SCN1A in all neurons. But they do show behaviors that resemble autism traits: They are less social and bury more marbles than wildtype mice do; and unlike wildtype mice, they show no preference for a novel object.
The reason seems to be that their VIP interneurons malfunction at a particular moment in cognition, as the researchers discovered when they dumped the excitatory neurotransmitter acetylcholine on brain slices from the mutant mice. The treatment simulates what happens in the brain when mice transition from an awake resting state to movement. Instead of exciting the interneurons, the VIP cells fired even less.
Similarly, the SCN1A mice showed reduced activity in VIP interneurons, specifically when the mice were transitioning from resting to running, Goldberg’s team found. By stimulating the interneurons optogenetically, the researchers were able to restore activity downstream, in the neurons involved in locomotion. The findings were published in June in Cell Reports.
The results suggest that a future treatment might include boosting VIP interneurons in people with Dravet syndrome at specific times to help with learning and attention difficulties, Goldberg says. Those treatments may be far off, but it’s a line of investigation his group is pursuing, he says — for instance, by trying to optogenetically restore the mice’s behaviors: “It’s kind of a first step in dissecting out cellular and circuit-specific bases of behavioral phenotypes of a very complex disorder.”
T
he study helps to “tease apart different mechanisms for different neurodevelopmental disorders, whether the epilepsy or autism,” says Kevin Bender, associate professor of neurology at the University of California, San Francisco, who was not involved in the new work. “The better we understand which particular cell types, the better we’re going to be able to understand how to target therapies.”The results could have implications for other forms of autism, Goldberg says. For example, malfunctioning VIP interneurons might underly features of autism in people who don’t have Dravet syndrome. Goldberg and his team have also found that some genes linked to autism are more strongly expressed in VIP interneurons than in other interneuron types or glutamatergic neurons.
That idea has promise, Bender says, because the disinhibitory effects of VIP interneurons are known to regulate top-down processes, such as attention and executive function, versus bottom-up processes, such as taking in sensory information. “One of the main theories of autism is that this bottom-up, top-down interaction has been disrupted,” he says. The fact that VIP interneurons malfunction here “is actually converging with other central theories or models of autism.”