Studies of tuberous sclerosis may shed light on biology of autism
Tuberous sclerosis provides a unique opportunity to understand autism because about half of people with that single-gene condition also have autism.
The genetics of autism is extremely complex, with mutations in any of several hundred genes conferring small amounts of risk. To slice through this complexity, scientists have focused on related conditions that are caused by mutations in a single gene. These conditions may point to common pathways among the various genetic causes of autism.
Tuberous sclerosis (TSC) provides a unique opportunity to understand autism because about half of people with that single-gene condition also have autism.
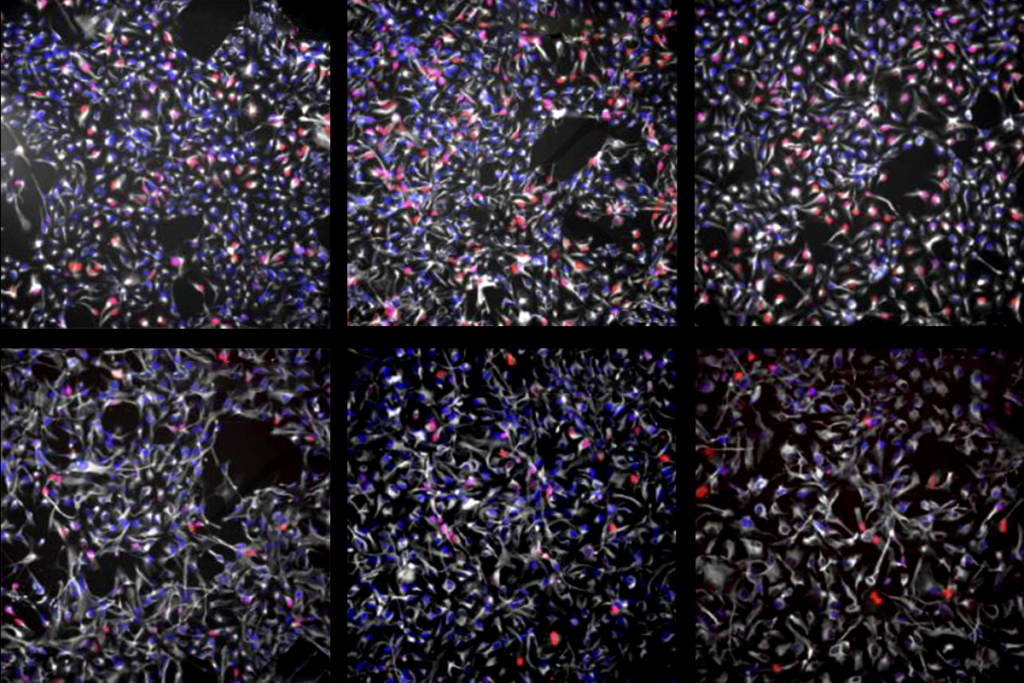
Caused by mutations in TSC1 or TSC2, tuberous sclerosis is a rare genetic condition characterized by non-cancerous tumors throughout the brain and body. The TSC proteins act as brakes on a key cellular enzyme, mammalian target of rapamycin (mTOR); when those brakes are gone, the mTOR pathway becomes overactive and cell growth can spin out of control.
Because mTOR is central to a wide variety of physiological functions, a whole host of researchers — those who study cancer, metabolism, immunology and neuroscience — are investigating this pathway. As a result, we probably know more about the mechanisms underlying TSC than those of any other single-gene condition associated with autism.
Also, researchers have detected altered mTOR activity in a number of genetic syndromes linked to autism, such as PTEN hamartoma tumor syndrome and fragile X syndrome. Targeting mTOR might improve outcomes in these conditions as well1.
Clinical trials in TSC have led to U.S. Food and Drug Administration approval of an mTOR inhibitor. The drug, everolimus, has positive effects on benign brain tumors, kidney lesions and seizures, although it does not seem to improve cognitive function or ease autism traits. Still, TSC can serve as a model for gene-specific, targeted treatment of conditions of brain development.
Early detection:
The ability to diagnose TSC at an early stage, coupled with an understanding of the genetics and cell biology of the condition, means that studying TSC could provide a unique window onto autism.
Clinicians often diagnose TSC before or around the time of birth — for instance, when they see a heart tumor in an ultrasound or echocardiogram. A fetus or newborn with multiple cardiac tumors has a 95 percent chance of having TSC. (These heart tumors usually disappear in time without treatment.)
In a 2017 multicenter study, researchers confirmed that cardiac tumors are the most common sign of TSC in the first year of life2. Thus, screening newborns for cardiac tumors provides a unique opportunity with which to investigate the development of autism — and possibly a window of time in which to intervene.
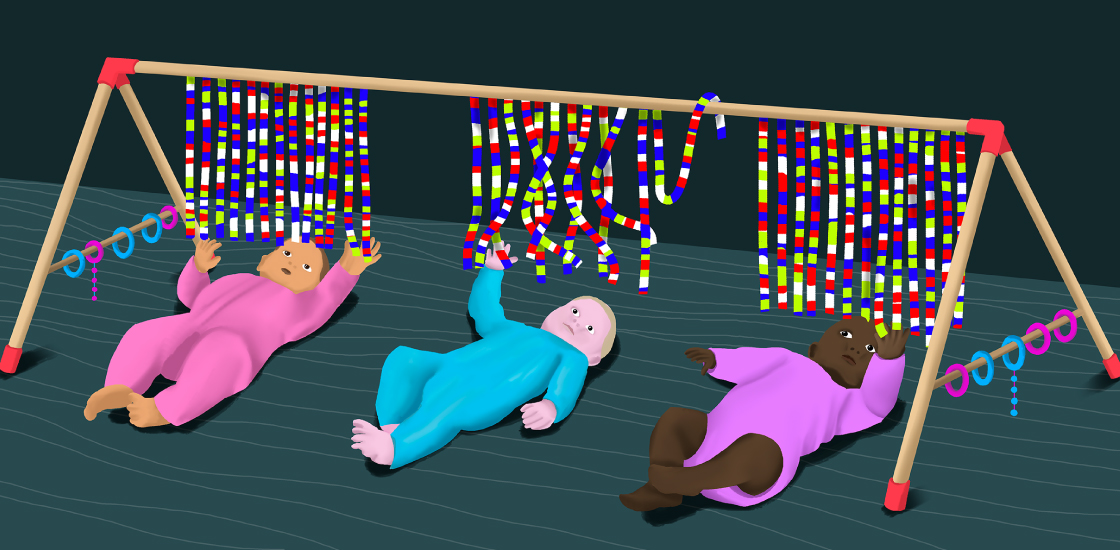
Because about half of newborns with TSC are later diagnosed with autism, we have the opportunity to ask a simple question: Can we predict which infants with TSC will receive an autism diagnosis?
Babies with TSC are an important study population. These babies have a higher risk of autism than do baby sibs — the younger siblings of autistic children, who stand a 20 percent chance of being diagnosed with autism. Researchers often study baby sibs to identify early biomarkers of autism, and children with TSC could be even more valuable, because they are more genetically homogenous.
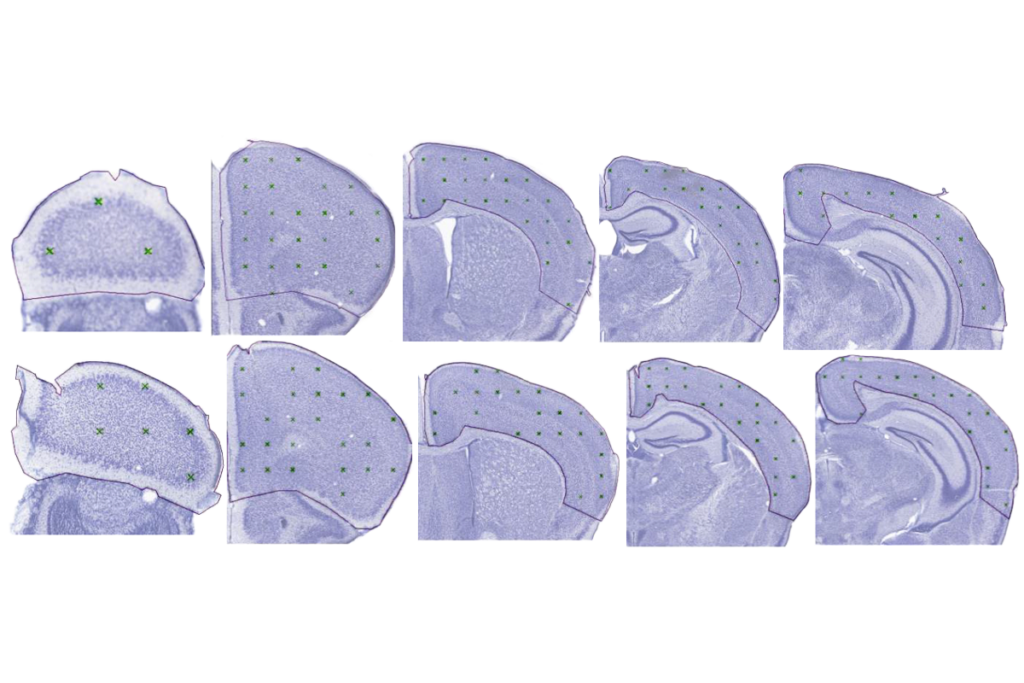
Studies of TSC mouse models may provide clues to which brain regions and neuron types are primarily involved in autism. Mice that lack TSC1 or TSC2 expression in the Purkinje cells of the cerebellum display autism-like traits, suggesting that the cerebellum plays a part in autism. And a study earlier this year showed that the pathway connecting the cerebellum to the ventral tegmental area, a brain region that encodes reward, is crucial for social preference in mice3.
These studies have led to the notion that changing the activity of the cerebellum using noninvasive means may have potential for treating people with TSC and autism4.
Treatment timing:
Treatment of autism features in TSC has not been straightforward, however. In a six-month trial, my colleagues and I did not detect any benefits of everolimus over a placebo for cognition or behavior in children and adolescents with TSC5. A European trial in similar age group also found that the drug does not seem to improve cognitive abilities or psychological function.
Age may have been a factor in the results: It may be difficult to modify behavioral circuits that have been hardwired for years. Studies in TSC mice support this idea. Treating TSC mice with rapamycin when they are 1 week old prevents both unusual social behavior and repetitive behaviors. Starting the treatment at 6 weeks of age normalizes social behaviors but not repetitive ones; and at 10 weeks, the drug has no effect on either measure6.
With this in mind, researchers are testing the seizure drug vigabatrin in infants with TSC. Trials with mTOR inhibitors given early in life are likely to be forthcoming.
Clinical trials of autism treatments have been stymied by a lack of informative biomarkers. A collaboration called the TSC Autism Center of Excellence Network has collected clinical data on more than 150 infants born with TSC, along with brain images, electroencephalography recordings and neuropsychological assessments. We hope the results provide clues to the roots of autism in TSC infants and point to brain signatures that foretell autism in infancy7.
I envision a day, not too far away, when newborns with TSC routinely undergo testing for brain signatures or other biomarkers that predict their risk of autism. The child could then begin behavioral and drug treatments early in life. That practice of prediction is likely to spread to, and greatly benefit, children with other conditions related to autism.
Mustafa Sahin is professor of neurology at Harvard University and director of the Translational Neuroscience Center at Boston Children’s Hospital.
References:
- Winden K.D. et al. Annu. Rev. Neurosci. 41, 1-23 (2018) PubMed
- Davis P.E. et al. Pediatrics 140, e20164040 (2017) PubMed
- Carta I. et al. Science 363, eaav0581 (2019) PubMed
- Stoodley C.J. et al. Nat. Neurosci. 20, 1744-1751 (2017) PubMed
- Krueger D.A. et al. Ann. Clin. Transl. Neurol. 4, 877-887 (2017) PubMed
- Tsai P.T. et al. Cell Rep. 25, 357-367 (2018) PubMed
- Williams M.E. et al. Am. Psychol. 74, 356-367 (2019) PubMed
Recommended reading

INSAR takes ‘intentional break’ from annual summer webinar series
Dosage of X or Y chromosome relates to distinct outcomes; and more
Explore more from The Transmitter
Xiao-Jing Wang outlines the future of theoretical neuroscience
Memory study sparks debate over statistical methods