For nearly three decades, Alzheimer’s disease has been framed as a story about amyloid: A toxic protein builds up, forms plaques, kills neurons and slowly robs people of their memories and identity. The simplicity of this “amyloid cascade hypothesis” gave us targets, tools and a sense of purpose. It felt like a clean story. Almost too clean.
We spent decades chasing it, developing dozens of animal models and pouring billions into anti-amyloid therapies, most of which failed. The few that made it to market offer only modest benefits, often with serious side effects. Whenever I think about this, I can’t help but picture Will Ferrell’s Buddy the Elf, in the movie “Elf,” confronting the mall Santa: “You sit on a throne of lies.” Not because anyone meant to mislead people (though maybe some did). But because we wanted so badly for the story to be true.
So what happened? This should have worked … right?
I would argue it was never going to work because we have been thinking about Alzheimer’s the wrong way. For decades, we have treated it as a single disease with a single straight line from amyloid to dementia. But what if that’s not how it works? What if Alzheimer’s only looks like one disease because we keep trying to force it into a single narrative? If that’s the case, then the search for a single cause—and a single cure—was always destined to fail.
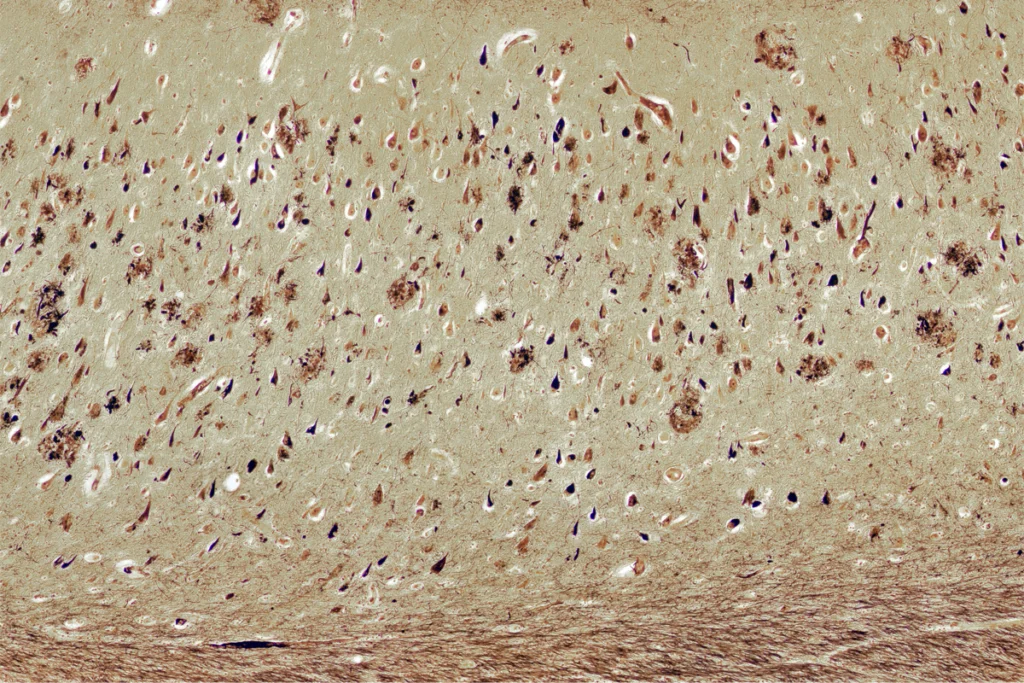
Real progress, I believe, requires two major shifts in how we think. First, we have to let go of our obsession with amyloid. Now don’t get me wrong. There’s no question amyloid plays a role. It was the first thing Alois Alzheimer saw under the microscope in 1906. And there’s decent evidence that misfolded amyloid spells trouble for the brain. But betting the house on clearing amyloid has been a costly mistake. In fact, we have long known that one-third of people with amyloid pathology do not show any cognitive symptoms, a disconnect that should have forced a rethink years ago.
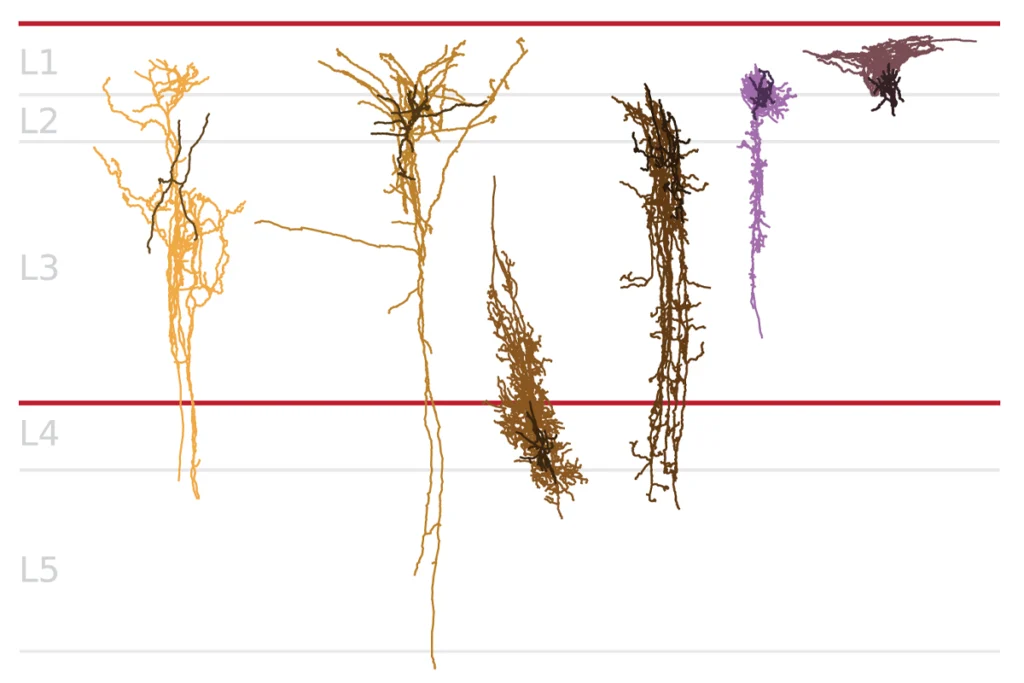
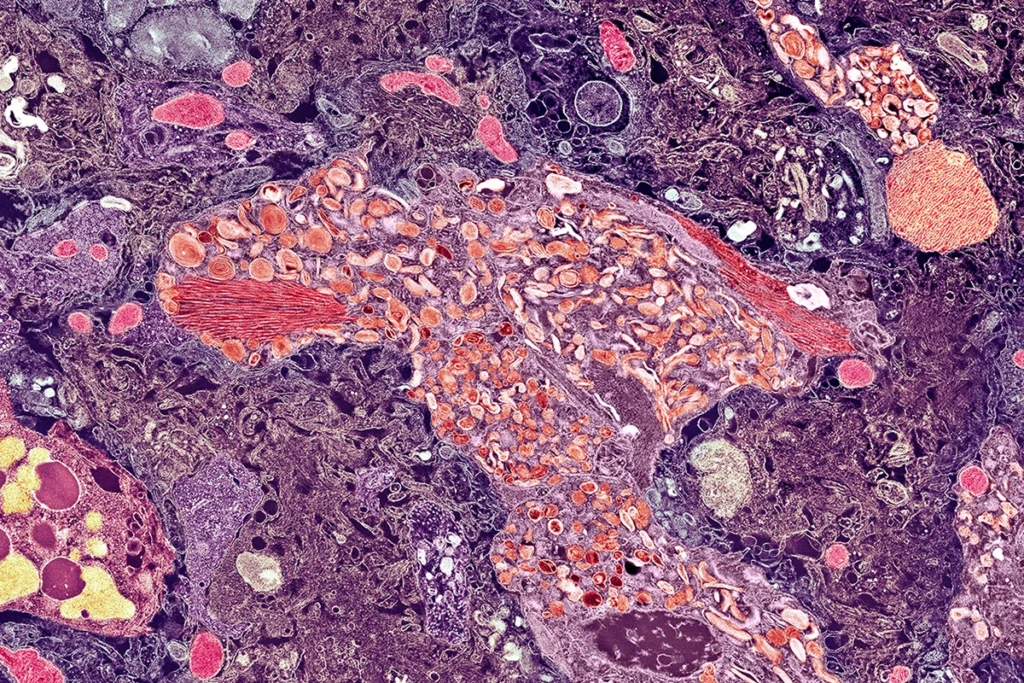
To the field’s credit, a shift is underway. We’re now exploring other mechanisms—tau, inflammation, metabolic dysfunction, vascular damage, neuronal hyperexcitability and more. But too often, these alternatives are still treated as side plots in an amyloid-centered story. They get less funding, less attention and fewer drug development efforts. That needs to change. These mechanisms may be far more central to the disease than we once thought. And they may drive it differently in different people.
This brings us to the second shift: We need to stop thinking in straight lines. The brain isn’t exactly a flowchart. It’s a dynamical system—a tangled web of feedback loops, compensations and nonlinear interactions. In such systems, small disruptions can ripple outward in unexpected ways. When one part starts to fail, another compensates. Over time, those compensations can become part of the pathology. In some people with Alzheimer’s disease, amyloid might be the trigger. In others, it might be inflammation, vascular injury, impaired glucose metabolism or runaway neural activity. These factors don’t act in isolation—they interact in complex ways, creating a web of multicausal loops. They are less like a chain of dominoes and more like a knot of tangled threads pulling on one another.
I
n systems terms, it’s not a cascade. It’s a state space. To understand this space, it’s useful to imagine a map in which every possible state of the brain is a point. In this space, healthy brains tend to move within a basin of attraction, a functional stable state. In Alzheimer’s, the brain may be pushed by interacting pathologies into a different region of state space, a pathological attractor—stable but dysfunctional.There’s growing experimental support for this view. Functional imaging, for example, has shown that people with Alzheimer’s spend more time in sparsely connected, low-flexibility brain states, and MEG recordings reveal changes in the temporal complexity of network dynamics. Recent work in my lab identified a dominant state, characterized by co-activity of nodes in the limbic network, that is linked to worse cognition and Alzheimer’s pathology. The idea is that once the brain tips into the dysfunctional state, it can get stuck there, even if you remove the original trigger.
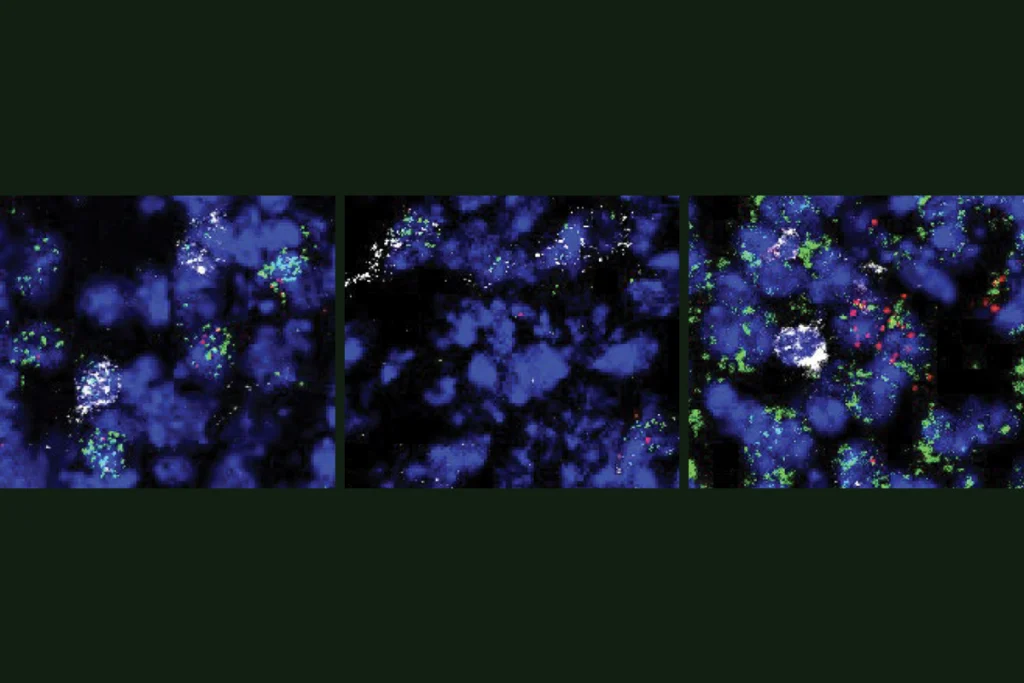
Researchers have already identified a number of “systems-level” factors that can disrupt network stability and contribute to Alzheimer’s disease, including vascular compromise, in which small vessel disease disrupts blood flow and triggers downstream effects; metabolic dysfunction, such as insulin resistance or glucose hypometabolism; runaway inflammation, such as overactive microglia or cytokine chaos; and overactivity, driven by an imbalance in neuronal excitation or inhibition. These factors may represent different systems-level routes to the same clinical outcome. Each person’s condition likely involves a different mix or “weighting” of underlying mechanisms. For someone with a history of diabetes, metabolic dysfunction might be the dominant factor. For someone with high blood pressure, the vascular component could play a bigger role. Ultimately, pinpointing this weighting—the primary mechanism driving the system’s dysfunction, or the mechanistic phenotype—could help match people with the most appropriate treatment.
This framing also changes how we think about treatment. In a system governed by feedback loops and nonlinear dynamics, removing a single trigger may not be sufficient to get the system “unstuck.” That may explain why anti-amyloid drugs haven’t made a major clinical impact: By the time symptoms show up, the system has already reorganized itself. Instead, we may need interventions that restore network stability—rebalancing excitation and inhibition, reducing inflammation or improving metabolic resilience. Noninvasive brain stimulation is one such approach, potentially nudging the system toward a more functional dynamic without needing to target a molecular mechanism. The goal isn’t to fix a part. It’s to shift the conditions that shape how the whole system behaves.
So where is amyloid in all this? Well, amyloid is always present, because our diagnostic criteria make it so. Think of it like background noise—it’s there, but it may not be what’s pushing the system off-key. Unlike the factors described above, amyloid doesn’t consistently drive network-level disruption. It reflects cellular dysfunction, such as misprocessing of amyloid precursor protein or altered lipid metabolism, but the downstream systems-level effects aren’t nearly as consistent or potent as those seen with, say, inflammation or synapse loss. This doesn’t mean addressing amyloid buildup or clearance has no clinical value. It just means it’s likely a small piece in a much larger puzzle. Focusing on it is like trying to fix a whole cacophonous orchestra by tuning but one violin.
Of course, there’s no perfect framework yet. To build it, we’ll need better tools. That includes better ways to capture brain dynamics in vivo, not just static pathology. We also need animal models that go beyond single-gene variants—instead, we need models that combine multiple hits, such as inflammation plus hyperexcitability. And we need ways to track these factors in humans, using multimodal imaging, physiological sensors and inflammatory biomarkers.
Getting there will take work. Paradigm shifts happen slowly, painfully, often after the old model has failed enough times to lose its grip. That’s where we are now. The dominant model isn’t working anymore. What comes next isn’t fully formed—but it’s coming into view. Mechanistic phenotyping and dynamical systems thinking may offer a path forward. It won’t be neat or linear. But it may finally meet the disease on its own terms.