An unaccounted confound lurks in functional MRI (fMRI) studies of psychedelics. The drugs alter neurovascular coupling, the assumed relationship between changes in blood flow and neuronal activity, according to a paper published in Nature Neuroscience earlier this month.
Over the past decade, fMRI studies have demonstrated that psychedelics disrupt functional connectivity in the default mode network and prefrontal cortex. But psychedelics don’t only alter neuronal activity, the new work reaffirms—they alter vascular activity, too.
Psychedelics activate the 5-HT family of serotonin receptors, which in turn constricts or dilates blood vessels. These vascular effects are baked into the etymology of the word serotonin: “serum” and “tone,” says study investigator Jonah Padawer-Curry, a postdoctoral fellow in Ted Satterthwaite’s lab at the University of Pennsylvania.
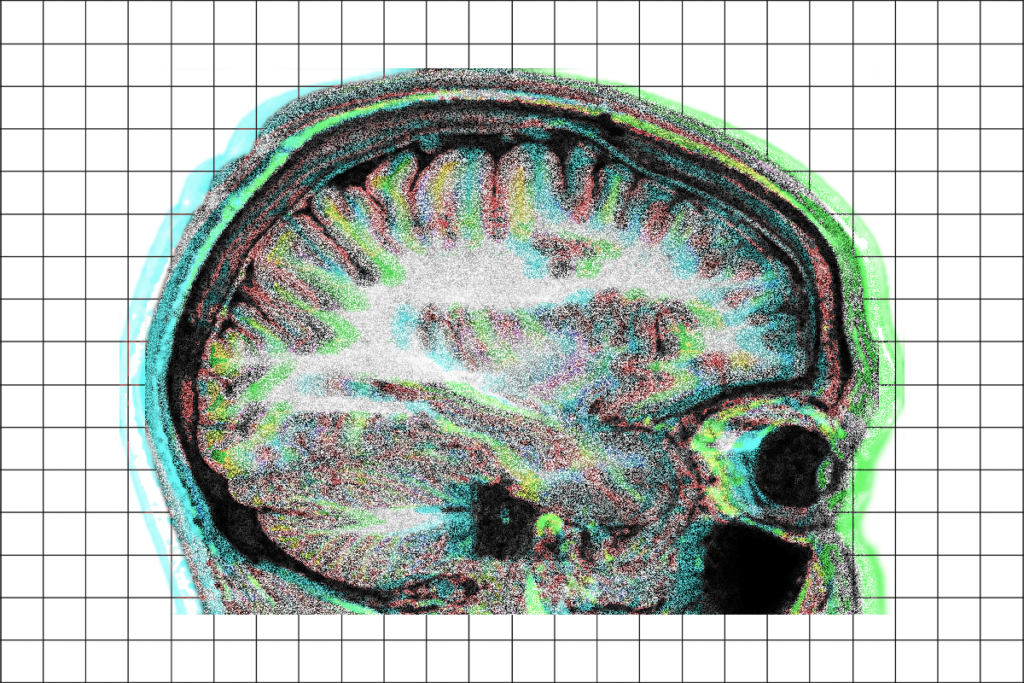
Researchers use fMRI to capture neuronal activity indirectly by tracking changes in blood oxygenation. Because neurons typically don’t store their own energy, they depend on the vasculature to provide them with oxygen and glucose through blood, says study investigator Adam Bauer, associate professor of radiology and biomedical engineering at Washington University in St. Louis. For this reason, changes in blood flow and neuronal activity should be coupled together.
“Trouble arises when we say that that relationship is constant across the brain,” and across people, ages and conditions, says Shella Keilholz, professor of biomedical engineering at the Georgia Institute of Technology and Emory University, who was not involved in the study.
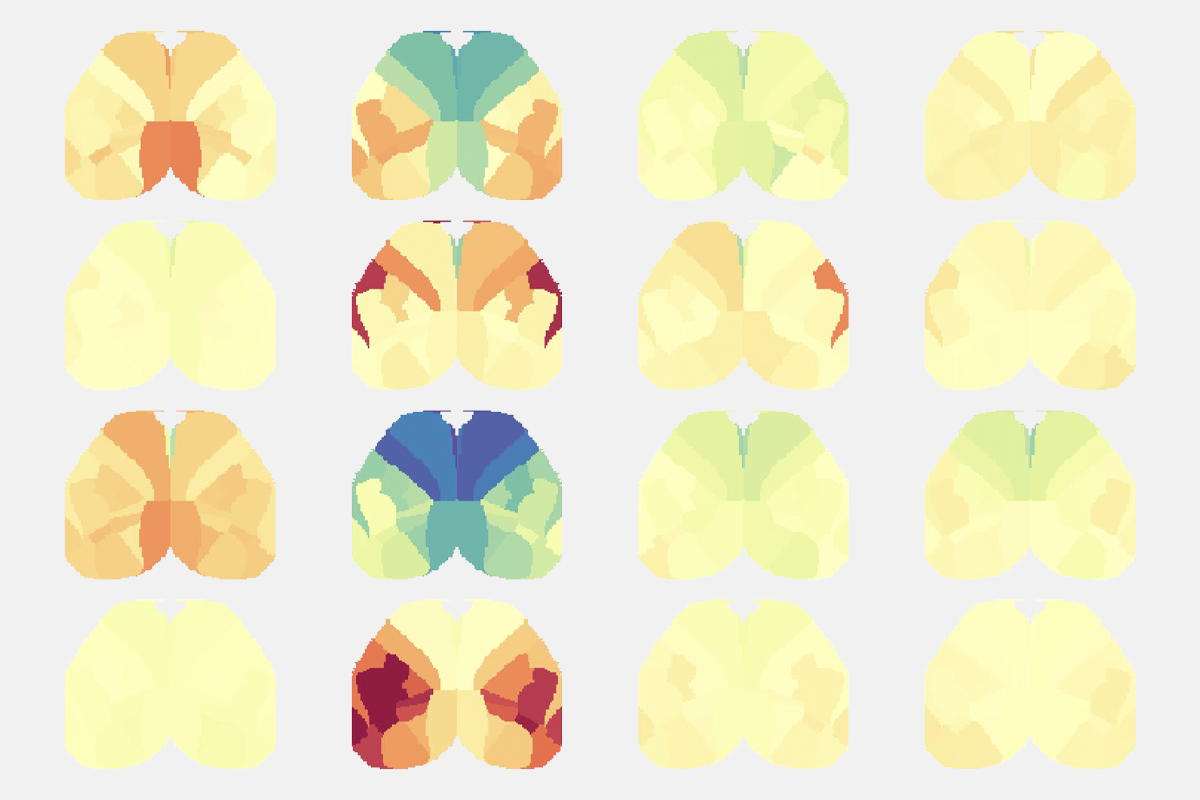
Bauer, Padawer-Curry and their colleagues gave the psychedelic 2,5-dimethoxy-4-iodoamphetamine (DOI) to mice and measured the resulting neuronal and hemodynamic activity changes using wide-field optical imaging. The drug, they found, modifies neurovascular coupling in different ways, depending on the brain region and during both the resting state and whisker stimulation. The team also uncovered potential signs of altered neurovascular coupling in data from a 2024 fMRI study that found psilocybin disrupts functional connectivity across the cortex.
The Transmitter spoke with Bauer and Padawer-Curry about what their findings mean for fMRI studies of psychedelics and how to best contend with this confound.
This interview has been edited for length and clarity.
The Transmitter: Why is it important to have a grasp on neurovascular coupling when conducting an fMRI study?
Adam Bauer: fMRI measures changes in oxygenation as a surrogate for neural activity. Inferences of neural activity through hemodynamic measures can be valid, as long as neurovascular coupling is intact. If you have deviations in coupling, you can’t necessarily keep talking about “this means that,” or even “this is linked to that.”
Jonah Padawer-Curry: I often think of it as like trying to determine what’s in a scene, but you’re only able to look at it through a camera. If the shutter speed or lighting changes, you’re now inferring that something in the scene changed simply because the measurement abstractly changed.
TT: How did DOI alter neurophysiology?
AB: The neuronal signal is not necessarily conveying the same change in activity as the hemodynamic signal, pre- and post-DOI. The changes in brain activity were very different in different regions. In some regions, we see increases in neuronal activity but decreases in hemodynamic activity, and vice versa. That’s what actually motivated us to model neurovascular coupling, because if we see disparity in which signals are changing and where, that immediately suggests that there’s decoupling between those two signals.
Some of the regions exhibiting the largest differences in neurovascular coupling were those that exhibited the largest disparities in changes in connectivity. If you were trying to understand how psychedelics affect brain organization, you’d get one answer by looking at hemoglobin and a different answer by looking at neuronal activity. The hemodynamic signal isn’t always relaying how the underlying neuronal activity is changing. And some of the regions with the largest changes in neurovascular coupling are the same ones consistently implicated in human fMRI psychedelics studies: the default mode network, including the posterior and anterior cingulate cortex, and the prefrontal cortex.
TT: What does that mean for interpreting changes in fMRI signal—should the previous studies be reevaluated?
AB: It’s entirely possible that these are the regions implicated in the effects of psychedelics and where structural remodeling takes place. That can absolutely be the case, but what we see is that there is disparity in what these signals are telling us; we see differences in signal changes depending on what we look at. We need to be cautious with the neuro-centric point of view of fMRI.
JP-C: I’ve thought a lot about that question from the broader philosophical perspective of what it means to measure brain function. The fact that a certain area in the brain is changing a lot—in neuronal activity and hemodynamic activity, even though they reflect different things—to me says there are changes in some underlying process that both of these signals measure. If you want to understand how the brain functions, whether or not you can say that measuring hemodynamics is also a measure of neuronal activity is a semi-moot point. Neuronal activity is not the only thing that makes the brain function.
Some people have asked me, “Oh, so are you saying fMRI is useless with psychedelics?” No, it’s just that your interpretation that everything is neuronal—how behavior is generated, how the brain functions—isn’t the right way to think about the brain. The solution is adopting a more holistic view.
TT: It sounds like asking how to mitigate these complications so that you can continue using fMRI to study neuronal activity is the wrong question.
JP-C: Right. Sometimes imposing constraints on a system is actually harder than relaxing those assumptions. We have to squeeze everything into this box to make sure that fMRI is measuring neuronal activity. But if we instead say that fMRI is measuring neurophysiology, a combination of many different parts of the brain, you’re actually less constrained in your interpretation of how the brain is changing.
AB: The way psychedelics affect the brain is complicated, and you can’t just get one result and cast it to a mechanism. Our results don’t mean that the default mode network isn’t affected by psychedelics. It’s that the changes in those regions give rise to differences in signaling, depending on the signal you look at. So at one level, that complicates things, but if the goal is to try to understand how these substances are affecting the brain, you might just need to use more tools. It’s not sufficient to use one modality to understand the system.
TT: Given that you found potential signs of altered neurovascular coupling in the 2024 study, do the conclusions of that work need to be reexamined?
JP-C: I don’t think our papers are in conflict with each other at all. fMRI is still an awesome measure. It’s still clearly measuring signals from the brain. It’s just that as soon as you invoke neuronal mechanisms—which, again, I think is the wrong standpoint—there’s going to be issues. I think study investigators Josh Siegel and Nico Dosenbach and their colleagues did a pretty good job of avoiding that.
AB: It’s an interesting thing that we see the largest changes in neurovascular coupling in the regions most often implicated with psychedelics, and we also see the most profound changes in functional connectivity in those regions, whether you’re looking at the neural signal or the hemodynamic signal. Perhaps the changes in neurovascular coupling are a part of the process.
JP-C: Neurovascular coupling certainly seems to be reflecting the change; I don’t know if it’s causing it. But the fact that all of these measures are in the same regions doesn’t falsify that they are important in the process. If anything, it almost bolsters the argument that that is a critical part of the brain for the acute and longitudinal effects of psychedelics.