Perimenopause: An important—and understudied—transition for the brain
Many well-known perimenopause symptoms arise in the brain, but we still know little about the specific mechanisms at play. More research—in both animals and humans—is essential.
The menopausal transition, or perimenopause, is a 2-to-10-year stretch of hormone irregularity leading up to menopause, when menstruation ceases permanently. It is a time that can come with a variety of challenging symptoms—including hot flashes, sleep disturbances and problems concentrating—as well as often underrecognized mental health challenges, such as heightened irritability, mood swings, increased anxiety and panic attacks. Importantly, a woman’s risk of depression grows two to five times higher than before or after the transition. Suicidal ideation and suicide rates in women are highest between the ages of 45 and 55.
What exactly is happening in the perimenopausal brain to trigger these increased risks? We know that perimenopause represents a major “neurological transition state”; the brain is exposed to drastically changing levels of ovarian hormones, similar to puberty but in reverse. As ovarian function declines, so do levels of the ovarian hormones estradiol and progesterone. The pituitary gland tries to compensate, resulting in erratic hormone fluctuations. These changes are sensed by the ovarian hormone receptors present throughout the brain, particularly in limbic areas important for emotion regulation and memory, such as the hypothalamus and the hippocampus. Neuroimaging studies in living humans have reported changes in estrogen receptor availability and brain metabolism across the menopausal transition.
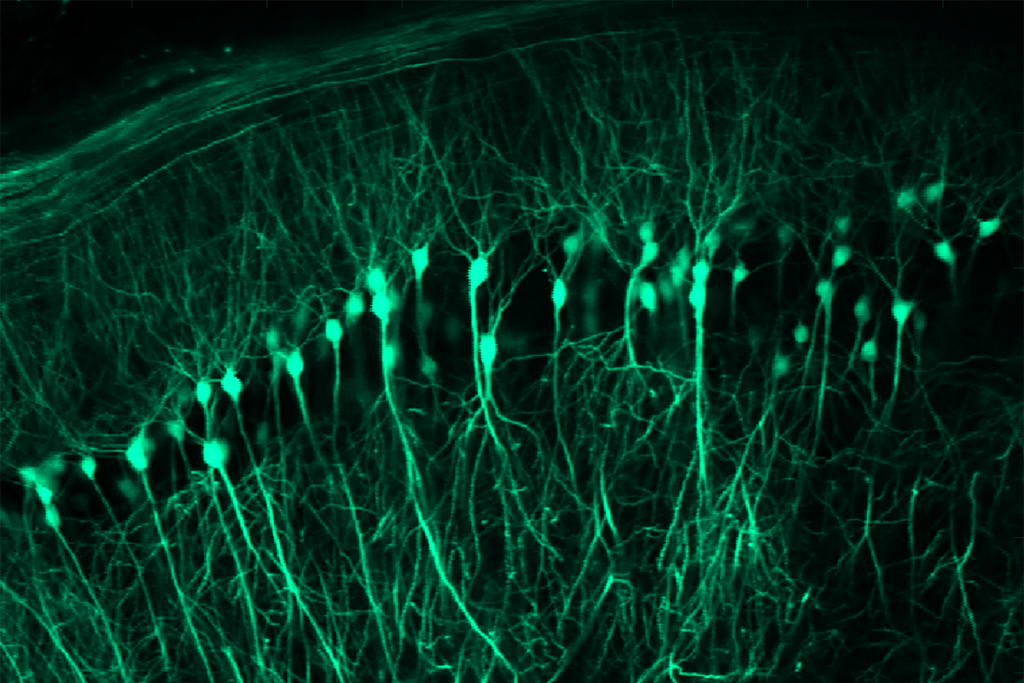
We also know that estradiol acts as a potent neuromodulator in the brain, affecting multiple neurotransmitter systems, including the serotonergic, noradrenergic and dopaminergic systems, and neuropeptides, such as brain-derived neurotrophic factor—all of which are known to be linked to depression and anxiety disorders. Mouse studies have revealed that hormone shifts across the ovarian cycle induce changes in chromatin organization that underlie changes in hippocampal gene expression, synaptic plasticity and anxiety-related behavior.
It seems likely that the mental health changes observed during perimenopause are related to the shifts in hormones and their receptors in the brain. Few studies, however, have explored the biological mechanisms underlying the increased psychiatric risk. Understanding these changes is essential both for developing new treatments for women in perimenopause who are experiencing mood and memory issues, and for understanding how these changes affect long-term brain health; metabolic changes during perimenopause are thought to increase the risk for Alzheimer’s disease, for instance.
B
ecause estrogen fluctuations or withdrawals drive the majority of perimenopausal and menopausal symptoms, menopausal hormone therapy is the treatment of choice, particularly for hot flashes and to prevent non-brain-related symptoms, such as osteoporosis. The therapy is not approved by the Food and Drug Administration for the treatment of perimenopausal depression, but some studies indicate that it may enhance the effect of antidepressants in perimenopausal women. However, given menopausal hormone therapy’s complicated history, not everyone chooses to take it, and it may be contraindicated in people who have had hormone-dependent cancers or cardiovascular disorders. Women sorely need more treatment options.A better understanding of the biological changes that underlie perimenopausal symptoms will help us get there. Take the case of hot flashes, one of the most common symptoms, affecting approximately 80 percent of women. They can lead to night sweats and difficulty sleeping, which can result in brain fog and lowered mood, initiating a vicious cycle. Indeed, studies have shown that more frequent hot flashes are associated with a higher risk of cardiovascular disorders, anxiety, poorer memory performance and depressed mood during perimenopause.
Hot flashes are brain based: Estrogen acts in the hypothalamus to control thermoregulation, and lower estrogen levels disrupt this process. Research in the 1990s on postmortem human brains identified a specific group of hypothalamic neurons that nearly doubled in size and showed higher expression of a peptide called neurokinin B in women after menopause. Mechanistic studies in rodents later found that targeting neurokinin receptors in these cells alters body temperature. This work eventually led to the first nonhormonal treatment for hot flashes: fezolinetant, a neurokinin 3 (NK3) receptor antagonist approved by the FDA in 2023.
This “bench to bedside” success story of the development of NK3 receptor antagonists for hot flashes offers hope that further study may lead to new and more effective treatments for other aspects of perimenopause. But studies of the molecular and cellular changes in the brain across the menopausal transition in humans are lacking—in part because this would require studies in postmortem human brains, for which information about menopausal status is typically missing.
To enable these studies, my lab has identified postmortem tissue biomarkers of the menopausal transition in blood, the hypothalamus and the pituitary gland. We believe that these new tools will have rippling effect on this field. We are using these markers to identify menopausal status in postmortem brain samples, and we plan to analyze changes in cellular composition, gene expression and chromatin in the human anterior hippocampus, which is involved in emotion and stress regulation. This study may deliver critical insight into the mechanisms underlying increased psychiatric risk and the interaction between shifting hormonal status and genetic risk factors for mental disorders during the transition to menopause.
The development of novel treatments, though, requires both human and animal studies. Mice do not menstruate and do not have menopause, but that should not prevent us from using mouse models to study the menopausal transition. In fact, hormonal profiles during the ovarian cycle in mice and humans are similar, even though the cycle lengths differ. To date, most rodent studies induce a menopausal-like state by removing the ovaries, which is a better model for sudden, surgically or medically induced menopause than for its natural occurrence. But newer approaches model ovarian hormone fluctuation using 4-vinylcyclohexene dioxide (VCD), a chemical that gradually depletes ovarian follicles, mimicking the natural transition in women. Both ovariectomy and the VCD model in rodents demonstrate that ovarian hormone fluctuations, and particularly estrogen withdrawal, can trigger anxiety- and depression-related behaviors. But understanding the causal molecular and cellular mechanisms in the brain will require further studies.
In sum, the menopausal transition is a challenging and underrecognized phase in life, with long-term consequences for brain health. More studies are absolutely critical for the development of new treatments and prevention strategies for perimenopausal symptoms and later health outcomes, but knowledge itself is empowering. The brain that knows of its transition is in a position to understand its options and make decisions to protect it long term.
Recommended reading

Sex hormone boosts female rats’ sensitivity to unexpected rewards
Neuroscience needs single-synapse studies
Explore more from The Transmitter
Spatial learning circuitry fluctuates in step with estrous cycle in mice
Why we need basic science to better understand the neurobiology of psychedelics