When a dangerous pathogen enters the body, the immune system gets to work, activating and recruiting cells and molecules to neutralize the intruder. But even before that happens, the brain appears to perceive potentially contagious people and prime the immune system to get ready for a possible infection, a study published today in Nature Neuroscience shows.
“We have this whole system for responding to real immune threats, but it seems you can probably utilize this network to respond to potential immune threats,” says Neil Harrison, professor of neuroimaging at Cardiff University, who was not involved with the study.
Thanks to the behavioral immune system, people can accurately identify someone who is sick and distance themselves or use other strategies to avoid exposure, previous studies have shown. And seeing pictures of people with visible symptoms of an infectious disease causes the observer’s white blood cells to release increased levels of proinflammatory molecules, a 2010 study found, suggesting that just the perception of sickness primes the immune system to respond more aggressively.
“What if [the brain] interacts with the immune system to prepare a reaction?” wondered Andrea Serino, professor of cognitive neuroscience at University Hospital of Lausanne, who led the new work. Serino had previously studied how the brain encodes peripersonal space—the dynamic representation of the world just beyond the body, where interactions with other people occur—and he suspected that representation could help a person sense danger even before exposure.
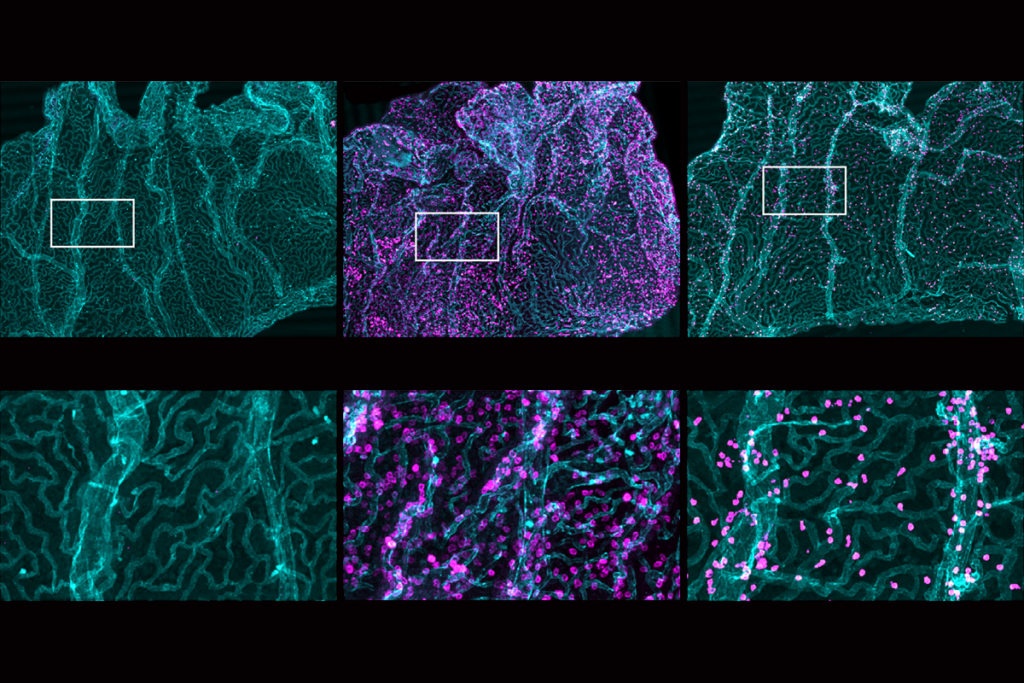
In the new study, when participants saw infectious avatars, modeled after actual infected people, their peripersonal space expanded, and associated brain regions were activated earlier than when they saw neutral or fearful avatars, Serino and his colleagues found. Seeing infectious avatars also activated specific brain networks associated with threat detection and switched on innate lymphoid cells in the periphery, teeing up a rapid response to any impending infections.
Even without contact, “the [central nervous system] is actually recognizing a threat and already priming the immune system to respond to that potential infectious threat,” says Michael Irwin, professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, who was not involved with the study. “That’s really novel.”
Still, the brain imaging experiments had small sample sizes, so the findings need to be replicated in larger and more diverse cohorts as well as in real-world scenarios to test their generalizability, Irwin says.
I
n one of the study’s experiments, 45 participants watched neutral, fearful or infectious avatars approach from different distances through a virtual-reality headset. At the same time, they received a light tap on the face and had to press a button as fast as possible when they felt the touch. (The team used this approach because the integration of visual and tactile stimuli helps to define a person’s peripersonal space.) Participants reacted most quickly to the face touch when they were viewing the sick-looking avatar, even when it was still relatively far away, suggesting it expanded their perception of their peripersonal space.These results make sense, Harrison says, because by the time an infected person gets close, it might be too late to avoid exposure.
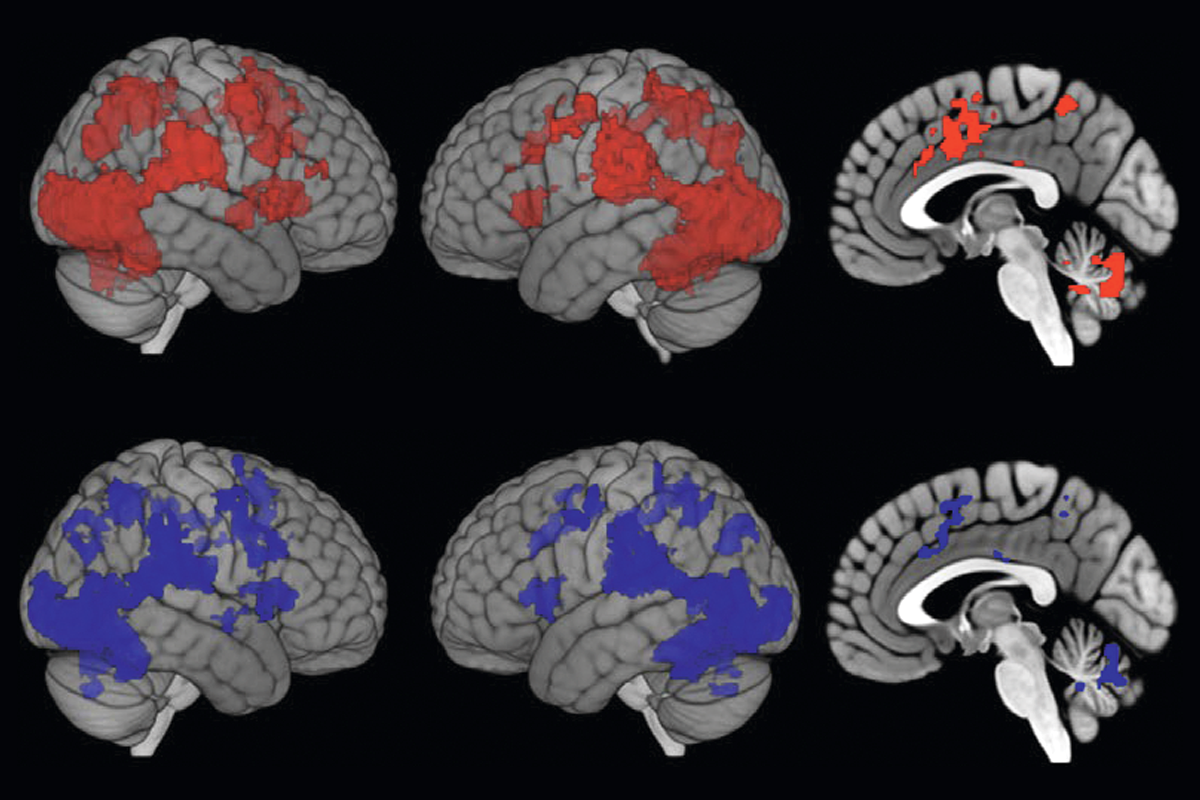
A separate cohort of 32 participants wore EEG caps as they watched the avatars. Seeing the infectious avatars turned on brain activity from farther away than neutral or fearful avatars, the imaging showed. Specifically, the infectious avatars activated areas related to the peripersonal system, such as the parietal areas.
The salience network, which filters out extraneous information to help a person focus on important stimuli, including threats, also turned on at the sight of the infectious avatars, according to a functional MRI experiment involving 38 additional participants. These brain areas and those related to peripersonal space connect more strongly to the hypothalamus in people exposed to infectious avatars compared with neutral ones. That suggests a link to the immune system, Serino says, because “the hypothalamus is one of the first layer[s] that can communicate to the immune system” through the hypothalamic-pituitary-adrenal cortex (HPA) axis.
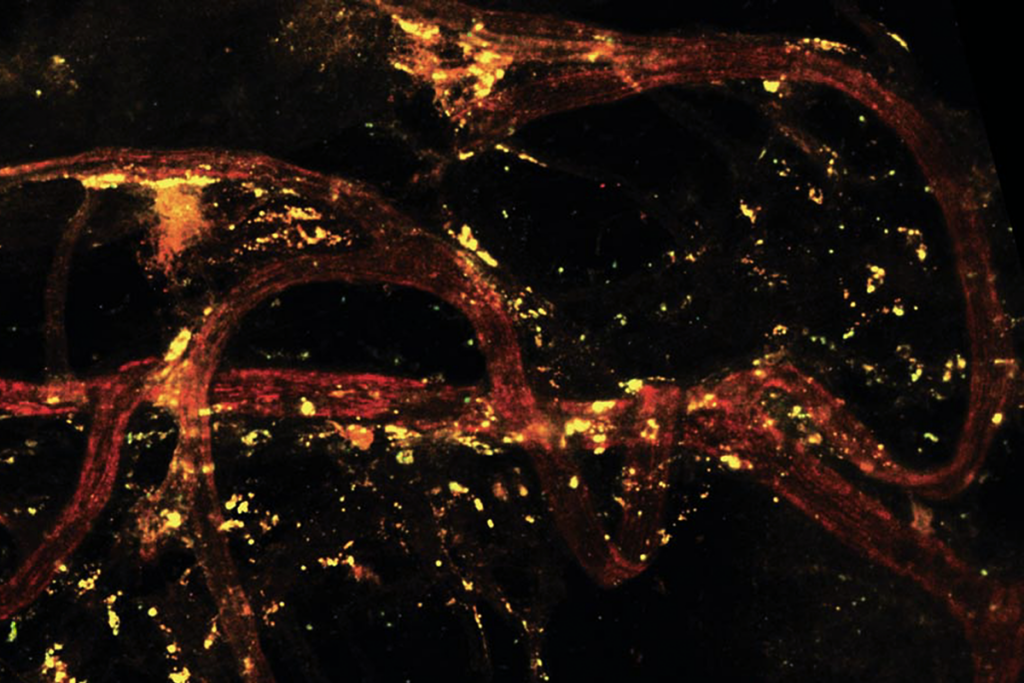
Indeed, immediately after exposure to the infectious threat, the numbers of various types of innate lymphoid cells changed, and the levels of immune activation markers increased. These results show that the “the immune system is intimately tied to the [central nervous system], and the recognition of threat is immediately translated to the immune system to produce a preparatory response,” Irwin says. The immune cell changes are similar to those seen in participants who received an influenza vaccine, the study shows.
As a final step, Serino’s team fed the data on the levels of hormones, lipids and neuroinflammatory molecules into a neural network and trained it to identify relationships among these measures and immune cell activation. This computational approach revealed that activation of the immune cells increased along with the HPA-related hormone and brain metabolite levels. The resulting model ties all of these systems together and suggests that increased brain activity in the hypothalamus drives the immune response, Harrison says.
“For a long time, we’ve sort of had the hunch that our brains respond to potential infective threats, but I think this study really does a very nice job in beginning to show how mechanistically that is enacted in the brain,” Harrison says. But because the study was done in a small population of young, healthy adults, and it is known that the immune and peripersonal systems vary with age, it remains an early step and will need to be replicated in diverse populations, he adds.
And although using avatars is an effective approach, “what I think is really necessary is to translate this virtual reality experience into an actual reality experience as much as you possibly could,” Irwin adds.
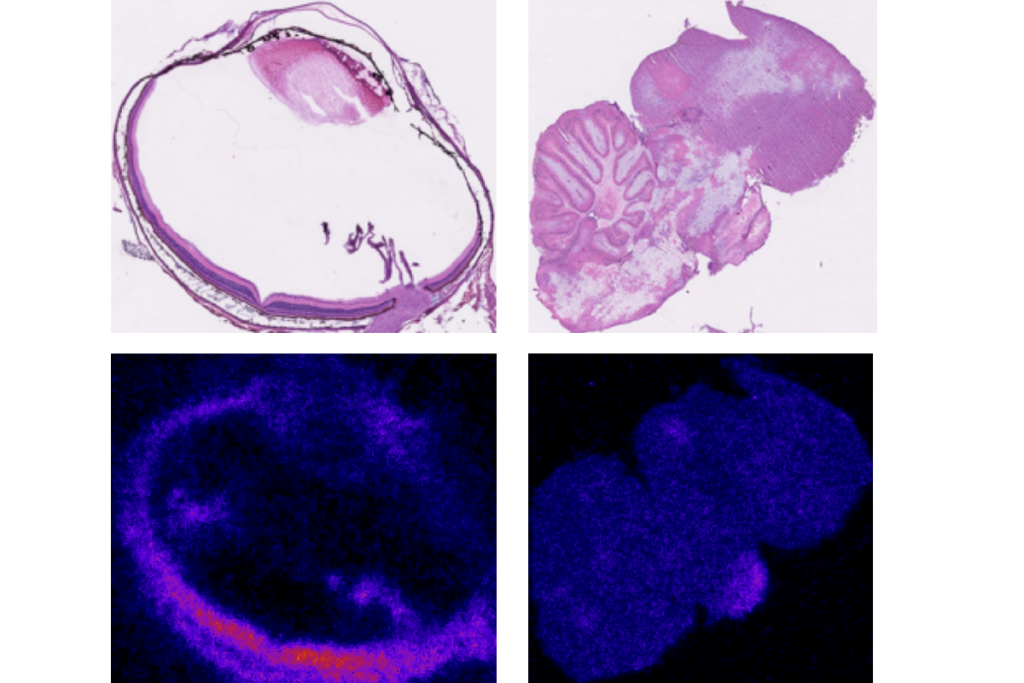
Because the brain imaging and blood measurements came from independent samples, Serino’s team is working to repeat and expand the experiments in a single cohort. The researchers are also putting sick mice close to healthy ones and analyzing the immune response and its connection to brain pathways.