How basic neuroscience has paved the path to new drugs
A growing list of medications—such as zuranolone for postpartum depression, suzetrigine for pain, and the gepants class of migraine medicines—exist because of insights from basic research.
Despite decades of basic research, many neurological and psychiatric conditions lack effective treatments, or at least treatments that work for everyone. For that reason, when I talk with colleagues about the value of research, I often hear the same negative refrain: “Basic neuroscience has not produced new drugs.”
Their argument carries some weight; many of today’s medications trace their origins to long-standing human use or to chance discoveries. The opium poppy, used for thousands of years to ease pain, paved the way for morphine and other opioids that are widely used as analgesics. Ketamine was designed as an anesthetic but was later unexpectedly revealed to be an antidepressant at low doses.
Yet this narrative is incomplete. It overlooks a growing list of medications—including zuranolone for postpartum depression, suzetrigine for pain, and the gepants class of migraine medicines—that exist only because of insights from basic research. These drugs were not stumbled upon or borrowed from traditional remedies. They were born out of a long arc of studies in the lab.
These success stories matter, because they demonstrate that neuroscience research can deliver new medicines. Acknowledging and publicizing such successes is especially important now, as public funding for basic research in the United States faces growing cuts and restrictions.
T
he development of zuranolone stemmed from an observation about allopregnanolone, a steroid our bodies naturally produce. It has little interaction with steroid receptors and instead acts on GABA receptors in the brain, making neurons less excitable. In the late 1990s, researchers reported that allopregnanolone levels in the rat brain rise dramatically during pregnancy, reaching concentrations of up to three times higher than normal. Just before giving birth, however, the level drops precipitously.From that finding came a bold idea: If the sudden crash in allopregnanolone levels triggers postpartum depression, restoring their levels could be therapeutic. The idea was put to test in clinical trials and ultimately proven correct. In 2019, the U.S. Food and Drug Administration approved brexanolone (Zulresso), a synthetic version of allopregnanolone delivered through infusion, the first drug approved specifically to treat postpartum depression. Two years ago, the FDA approved an oral version called zuranolone (Zurzuvae).
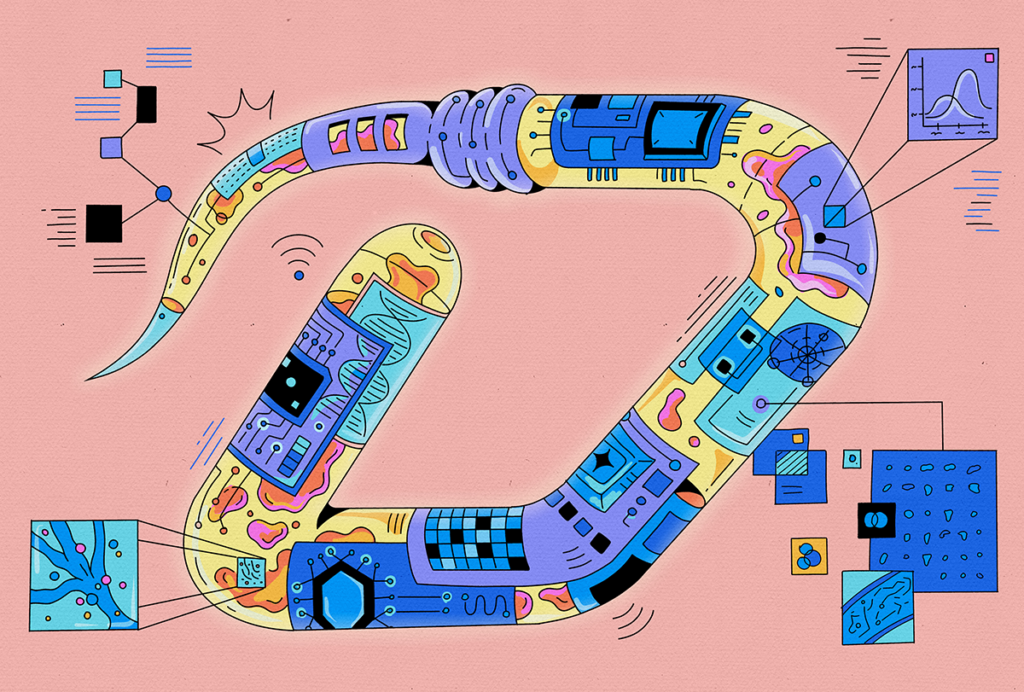
A new, non-opioid pain drug similarly emerged from basic neuroscience research. Pain signals begin in sensory neurons in the dorsal root ganglion. To transmit sensory information to other cells in the nervous system, these neurons fire action potentials that depend on sodium channels opening in the cell membrane. In a 1996 rat study, scientists reported that these sensory neurons possess not only the usual sodium channels but an extra type called Nav1.8. Without Nav1.8, sensory neurons can produce a few action potentials but cannot sustain firing.
Because Nav1.8 expresses mainly in the dorsal root ganglion and not elsewhere in the brain, the channel offers a way to block pain transmission without impairing brain activity. And because Nav1.8 is a completely different mechanism than opioid receptors, targeting the channel doesn’t come with the addictive potential of opioid drugs. Building on this insight, Vertex Pharmaceuticals developed suzetrigine (Journavx), a small molecule that selectively blocks Nav1.8 for pain management, approved by the FDA earlier this year as a short-term treatment for moderate to severe pain.
Similarly, a peptide discovered in the 1990s called calcitonin gene-related peptide (CGRP) inspired a new class of migraine therapies, offering hope for those who don’t respond to existing therapies. Rat trigeminal neurons produce CGRP in abundance. One branch of these trigeminal neurons wraps around the brain’s large arteries. When activated, the nerve releases CGRP, stretching the vessel walls, further stimulating the nerve endings, triggering a vicious feedback loop that transmits relentless pain signals to the brainstem.
The FDA approved the first CGRP receptor blockers, ubrogepant (Ubrelvy) in 2019, followed by a wave of similar drugs. Several anti-CGRP monoclonal antibodies are used for migraine prevention. Unlike older migraine medications, which can pose risks for people with hypertension, the new CGRP-based treatments work through a different mechanism. They offer a safer and effective option to manage migraines.
Other examples show how neurobiology has driven drug discovery. Studying how hypothalamic neurons regulate body temperature resulted in a first-of-its-kind drug, fezolinetant (Veozah), for reducing hot flashes and night sweats in women going through menopause. Targeting the N-type calcium channel led to ziconotide (Prialt), a treatment for chronic pain. And perhaps the best-known case: Recognizing a deficiency of dopamine in people with Parkinson’s disease led to L-DOPA, still a commonly used treatment. Beyond discovering new mechanisms, basic research has also guided us toward drugs with better distribution in the brain and fewer side effects.
I
t’s fair to ask why, given decades of basic neuroscience research, there aren’t more examples of these sorts of success stories. The answer is complicated. Even if we get the biology right, drug development can fail, whether due to soaring costs, flawed trial design or unwanted side effects. But we can help spur the hit rate by thinking about ways to improve translation, and by looking for lessons from previous successes.Progress often comes from digging deeper into biology, like when scientists identified CGRP, which created a new drug target. Though animal models of brain disorders have helped validate findings, they may not be the best place to discover targets. Indeed, sometimes the most powerful clues come from simple measurements of the nervous system, such as allopregnanolone levels during pregnancy. In many cases, we may not need to fully understand the complex causes of a disorder but rather just find the right place to intervene, as targeting Nav1.8 in sensory neurons showed for pain. Finally, progress has been faster for conditions that are more clearly defined. Depression covers a wide spectrum of symptoms. Postpartum depression, by contrast, offers a more focused entry point, which made it easier to find an effective treatment.
The recent success stories also drive home a crucial point: Translation takes time. Each of the breakthroughs I’ve described began with discoveries made in the 1980s and 1990s, yet only in the last few years have approved treatments become available to patients. That history proves what basic neuroscience can deliver. And with the pace of discovery accelerating over the past two decades, I believe we are on the verge of seeing more basic discoveries transformed into new medicines. Of course, realizing this promise depends on sustained public investment in basic research. We need the basic neuroscience discoveries to drive the future medical breakthroughs.
AI use disclosure
Recommended reading
Let’s teach neuroscientists how to be thoughtful and fair reviewers
Lack of reviewers threatens robustness of neuroscience literature

Dendrites help neuroscientists see the forest for the trees
Explore more from The Transmitter
Whole-brain, bottom-up neuroscience: The time for it is now
Why we need basic science to better understand the neurobiology of psychedelics