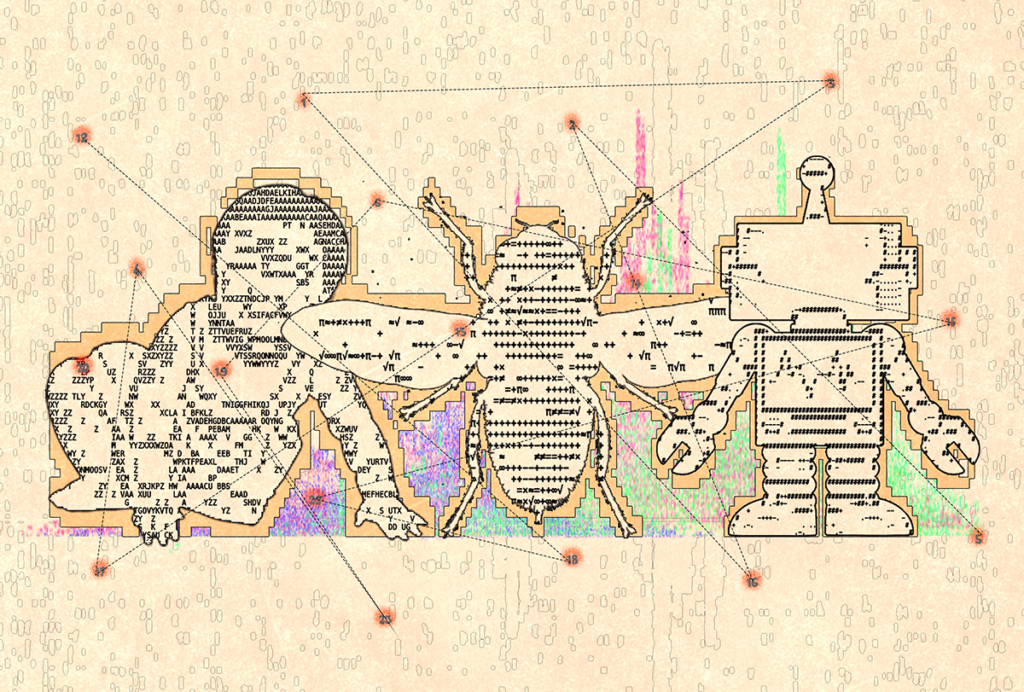
Getting at the heart of autism
Cardiac activity could reveal autism’s physiology and confirm a hunch many clinicians share: that people with autism experience great stress.
A
loud, unexpected gurgle from your stomach, an uncontrollable urge to yawn, a galloping heartbeat before a big presentation. These disparate bodily activities — digestion, sleep, stress — all come under the purview of your autonomic nervous system, a network of nerves and fibers that extends to almost every organ in your body.Like the autopilot in an airplane, this system constantly makes subtle adjustments to your physiology in response to your surroundings. If you confront danger, the ‘sympathetic’ arm of the system revs up your circulation to prepare you to fight or take flight. By contrast, when you need to rest or digest, the ‘parasympathetic’ branch kicks in, relaxing your organs and muscles.
The wrong response, meanwhile, can have serious consequences. If your body stays primed to face danger for too long, for example, the familiar may seem frightening. Remaining in this state can also lead to anxiety, problems with social interactions and sleep, even heart and digestive troubles.
These conditions are all associated with autism, and so — no surprise — the idea that the autonomic nervous system is intricately involved in autism has caught the attention of a number of researchers. There is even some evidence that autistic people have trouble anticipating changes in their environment and are less likely to habituate to background sounds or repeated events. “There are a lot of reasons to believe that individuals with autism experience the world in a less predictable and more overwhelming way,” says Matthew Goodwin, an experimental psychologist at Northeastern University in Boston, Massachusetts.
Goodwin became interested in the autonomic nervous system as an undergraduate student in the late 1990s. At the time, he was exploring whether people with autism experience stress more often or more acutely than typical people do. “The task that I was put forth was: ‘How do we measure stress?’” he says.
At first, Goodwin set out to understand how autistic people respond to everyday stressors, such as a loud noise. But some of his participants were minimally verbal and could not readily express how they felt. So he decided to collect their physiological measurements as well.
The work was slow-going. The participants often had unexpected meltdowns, throwing off all of the data Goodwin had collected in a session. But as he paired videos of these episodes with the physiological measurements, he began to realize that his problem presented an opportunity: Just seconds before an autistic participant had an outburst, their physiology also changed. “It’s been my crusade” ever since, he says, to try to predict behavior based on these shifts.
Goodwin is one of several researchers studying autonomic function in autistic people. Their preliminary findings suggest that there are compelling differences, particularly in the variation in heart rate, between autistic people and their neurotypical peers, but the reasons for those differences are still unclear. It might be that the fraught way in which some autistic people experience the world shapes their autonomic nervous system to be less flexible than usual, and to linger in a high-stress state.
But there could be a deeper connection between the system and autism, too: Autonomic dysfunction might give rise to many traits associated with the condition. A lack of flexibility in how the body regulates physiological states could explain many autism traits — including social challenges, emotional outbursts, sensory sensitivities, restricted and repetitive behaviors and speech-processing difficulties, argues Stephen Porges, professor of psychiatry at University of North Carolina at Chapel Hill.
Although his theory is not widely accepted, “from my perspective, it requires a total reconceptualization of what the disorder is,” Porges says. “There has to be an understanding that much of the behavior that we’re calling autism is really due to the body of the individual being in a state of defense.”
Flex benefits:
R
esearchers have been trying for years to pin down patterns linking autism and the autonomic nervous system. Part of their challenge has been that there are many facets of autonomic regulation to measure, including skin temperature, heart rate, blood flow, sweat, and even liver and gut activity.Over the past 50 years, autism researchers have studied at least eight indices of cardiac function alone, including heart period, the interval between beats; heart rate variability, or the variation in heart rate; and respiratory sinus arrhythmia, or the variability in how heartbeat and breathing sync up. Some, such as heart rate variability, can be calculated in multiple ways.
This wide range of possible measurements — as well as advances in how they are taken — has led to conflicting results. But in the past five years, some findings are starting to be replicated by independent groups, says Michelle Patriquin, assistant professor of psychiatry and behavioral sciences at Baylor College of Medicine in Houston, Texas. “I think that starts to make people really take notice.”
Of all the autonomic signs researchers have tracked, heart rate variability — and its related measure, respiratory sinus arrhythmia — may be most relevant to autism, she says. “It seems to be the most powerful [index], and the most correlated to emotional and behavioral outcomes.”
Scientists have theorized that a higher heart rate variability goes along with a more active parasympathetic nervous system, in which the body’s organs are better able to relax. The theory holds that the variation in time between heartbeats is lowest when we’re stressed. (In a state of panic, after all, heart rate typically shoots up and stays elevated until we calm down.) By contrast, variability is high when we’re relaxed.
Some studies have shown that a lower heart rate variability is tied not only to autism, but also to depression, psychosis and schizophrenia. “Heart rate variability has been used as a health index measure across a range of physical and psychological disorders,” says Adam Guastella, professor and clinical psychologist at the University of Sydney in Australia, who has done some of this work.
Guastella’s team has found that, among typical people, heart rate variability can reflect an individual’s facility for reading another person’s emotions: The lower the variability, the weaker the ability to recognize social cues. In 2015, Guastella and his colleagues conducted a meta-analysis of 13 studies that also linked increased heart rate variability to better social skills and decreased stress in nearly 800 typical participants. They have also found that giving people oxytocin, a hormone associated with social bonding, can increase their heart rate variability.
In people with autism, too, several studies have hinted that lower heart rate variability tracks with poor social skills and intellectual impairment. One 2016 study found that autistic teenage boys with greater social challenges have lower respiratory sinus arrhythmia than do those who have better social skills.
A highly variable heart rate may reflect an autonomic system that is more responsive to changes in the environment. The more responsive the system, the more biological support the person has in adapting to a given situation, says Sara Webb, professor of psychiatry and behavioral sciences at the University of Washington in Seattle. “You’re regulating all of these physiological ways that your body works, so that you are really in the best state to perceive your environment.”
On a television screen in Webb’s lab, a video shows otters drifting in the water, then a string of penguins waddling over the ice. The soft sounds of instrumental music play in the background. A 2-year-old girl stares at the scene, transfixed.
She is sitting in a highchair, with seven or eight sticky sensors trailing down her back. Each sensor is attached to a long, thin cable that connects to a small receiver, which she wears in a backpack. The receiver transmits wirelessly to a computer that collects physiological data, including the girl’s heart rate. The setup is meant to capture something similar to a ‘resting state’ in children, Webb says, but she adds with a laugh: “Children are always being stimulated; they don’t rest.”
Webb and her colleagues used this setup to study heart rate variability in 137 toddlers, 71 of whom have autism. But after two sessions with each child, they found no difference, on average, between the two groups.
That might sound like a blow to the theory that autonomic differences exist in autism. But when the team took a closer look at only the autistic children in their study, they found patterns within the group: In particular, higher heart rate variability tracked with greater language ability.
And Webb offers an explanation for the lack of differences between groups: It may be that autonomic differences arise only in certain situations — such as when a child is presented with a particular task. In a follow-up study, Webb’s team plans to look at children during learning, a scenario in which different autonomic states might be especially useful. A little flight-or-fight energy might aid a test-taker, for instance, whereas a state of calm would better serve someone trying to master a new concept.
Along those same lines, Patriquin has found autonomic differences among 23 autistic children, aged 4 to 7 years, confronted with social tasks: Those with greater respiratory sinus arrhythmia, which is linked to higher heart rate variability, also have better social skills, joint attention and language abilities. “You have to have a certain physiological state in order to be able to engage effectively,” she says. “If you’re in flight-or-fight mode, you might stutter; your language might change; your voice might get shaky, or you might not even speak at all. ”
And the beat goes on:
T
here may be another reason why the typical and autistic toddlers in Webb’s study showed only negligible differences in autonomic function: The differences may only become apparent over time. “I do wonder whether life experiences and anxiety throughout life have an impact on overall heart rate variability,” says Tessel Bazelmans, a research associate at King’s College London who works with Webb. Confirming this idea calls for a study that would follow people over many years.No such study exists in autistic people, but there are studies that offer snapshots in time. At least one study shows that in adulthood, autistic people have lower heart rate variability than their typical peers. And in a study published in March, researchers tracked heart rate and respiratory sinus arrhythmia in 118 children, 12 of whom have autism. Between the ages of 1 month and 6 years, all of the children showed a decrease in heart rate and an increase in respiratory sinus arrhythmia. After 18 months, though, the increase in respiratory sinus arrhythmia slowed in the autistic children.
“The children with autism basically fell off the more typical developmental growth curve,” says lead investigator Stephen Sheinkopf, associate professor of psychiatry and human behavior at Brown University in Providence, Rhode Island.
Toddlers who score below average on tests of social responsiveness show a similar plateau or delay in the rise in respiratory sinus arrhythmia, according to a study by Patriquin and her colleagues. In a follow-up analysis, that group also found decreased respiratory sinus arrhythmia among 4-year-olds who showed behavioral problems. None of the children in either study had an autism diagnosis, but they were socially withdrawn or aggressive, both of which are linked to the condition.
This divergence in trajectories between typical children and those with autism traits is subtle, but it could be significant: The split coincides with the age at which autism traits often surface. And it reinforces the theory that the autonomic system is altered in autism. “It can raise various hypotheses,” Sheinkopf says. In contrast with Porges’ ideas, Sheinkopf’s theory suggests that the period when autism traits appear is especially challenging for children, ramping up their stress response — and autism traits would lead to elevated flight-or-fight reactions.
Given how heterogeneous autism is, researchers may never be able to demonstrate clear autonomic differences between autistic and typical people. But scientists are plumbing the possibility that heart activity could serve as a marker of well-being and social function in autistic people. If, for example, it turns out that autonomic functioning tracks in a consistent way with social behavior, researchers could measure heart rate variability to assess the success of social-skills training. That approach would be especially beneficial for individuals with limited verbal abilities.
Autonomic differences might also help clinicians make behavioral predictions in this group. Goodwin and his colleagues have tested a wristband device that tracks heart rate, skin temperature and sweat. In June they reported that, using those data, they can accurately detect an autistic person’s aggressive outburst a minute before it happens 84 percent of the time. It’s not yet clear how best to use that warning, Goodwin says, but “if we only ever can do 60 seconds, it’s [still] a lot.”
Tracking autonomic function might also put repetitive behaviors in a new light. Specifically, it might help to confirm — or refute — the idea that ‘stimming,’ repetitive movements such as rocking or hand-flapping, helps autistic people to self-soothe: Heart rate data might confirm their state of calm or agitation much better than any other available tools.
Analyzed early enough, autonomic data could even signal autism earlier than all diagnostic tools in use now. “My dream is to do a study in utero, where you start to measure heart rate variability for high-risk babies,” Patriquin says. Infants with low variability in their heart rate might benefit from ‘kangaroo care,’ in which caregivers hold their babies against their bare skin for prolonged periods. Some research suggests the intervention can modify autonomic functioning.
Similar approaches might help adults, too. Porges has pioneered the ‘Safe and Sound Protocol,’ which uses music to try to lower stress. He has started testing in autistic people. “If you can intervene and get that physiological state calmer or safer, spontaneous social behavior occurs,” he says.
If nothing else, autonomic measures might offer a detailed glimpse into the experience of having autism, Patriquin says. A spike in heart rate or shift in breathing can offer, as she says, “a clearer picture of what their internal life is like.” Family members, clinicians and teachers could get a better understanding of what an autistic person experiences, and not just what they show through their behavior, she says: “There’s stuff going on inside that’s different; they feel different.”
Corrections
A previous version of this article mistakenly referred to autistic meltdowns as tantrums; the two phenomena are distinct.
Recommended reading

Poor image quality introduces systematic bias into large neuroimaging datasets
Probing the link between preterm birth and autism; and more
Cell ‘antennae’ link autism, congenital heart disease
Explore more from The Transmitter
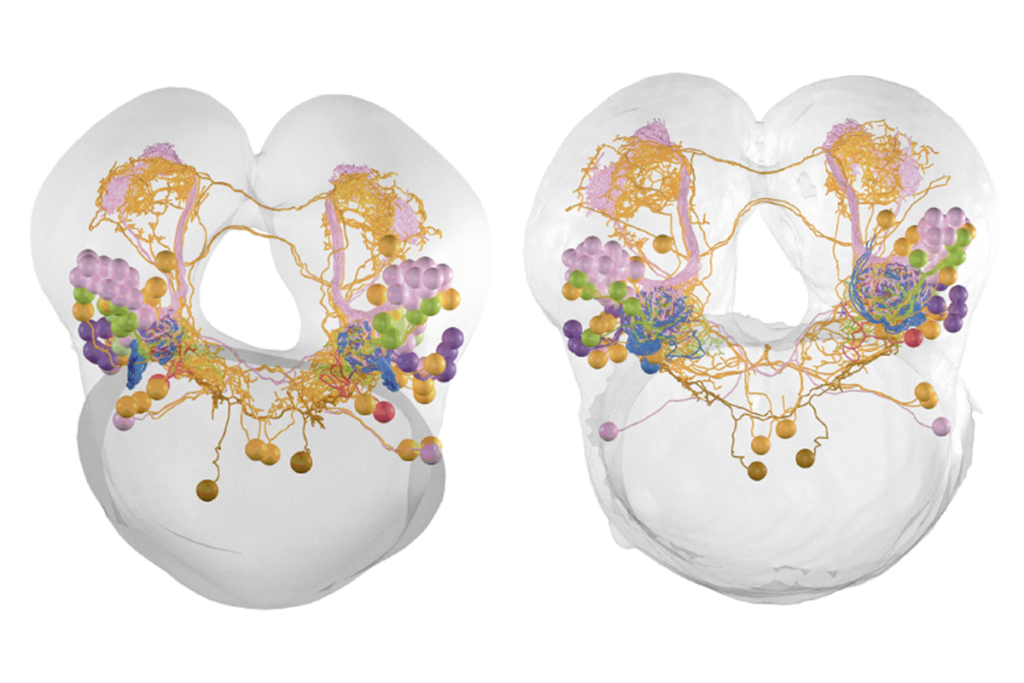
Cross-species connectome comparison shows uneven olfactory circuit evolution in flies
Null and Noteworthy: Downstream brain areas read visual cortex signals en masse in mice